Shocking New Study Reveals Gastroesophageal Reflux Disease (GERD) May Secretly Threaten Your Heart Health!
2024-11-19
Author: Wei Ling
Introduction
A groundbreaking study recently published in the Journal of Translational Internal Medicine has unveiled startling new insights into gastroesophageal reflux disease (GERD) and its potential connection to cardiovascular health. Traditionally viewed merely as a digestive ailment characterized by persistent acid reflux and uncomfortable heartburn, this condition may have implications for heart disease and overall cardiovascular well-being.
Study Methodology
Using a comprehensive bidirectional Mendelian randomization (MR) approach, researchers have presented compelling evidence that GERD could significantly influence critical cardiovascular risk factors, including blood pressure levels, lipid profiles, and even the likelihood of developing heart disease. "Our research emphasizes that GERD impacts cardiovascular risk in a significant manner, offering a more holistic perspective on its health implications," stated Qiang Wu from the Senior Department of Cardiology at the Sixth Medical Center of the Chinese PLA General Hospital in Beijing.
Robust Methodology
What sets this study apart is its robust methodology, which leverages genetic data to draw causal connections, effectively controlling for confounding variables and the potential for reverse causation—making the findings more reliable. Researchers analyzed genetic variants linked to GERD and utilized these as instrumental variables to explore how GERD could causally affect cardiovascular health, as highlighted by Qiang Su from Jiangbin Hospital in Guangxi.
Study Scope
The vast study examined a two-sample MR approach, gathering data from genome-wide association studies (GWAS) involving over 600,000 participants, including 129,000 individuals diagnosed with GERD. The cardiovascular data came from an additional cohort of more than 200,000 Europeans. Key metrics such as systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (PP), and mean arterial pressure (MAP) were scrutinized.
Findings
Employing advanced MR methods such as Inverse Variance Weighted (IVW) analysis and MR Egger regression, the researchers effectively controlled for pleiotropic effects—where one gene affects multiple traits—enhancing the credibility of their conclusions. Notably, genetically predicted GERD correlated with heightened blood pressure, demonstrating a significant relationship where SBP was elevated (β = 0.053, P = 0.036) alongside DBP (β = 0.100, P < 0.001). This raises alarm bells as increased blood pressure is a well-known precursor to heart disease and stroke.
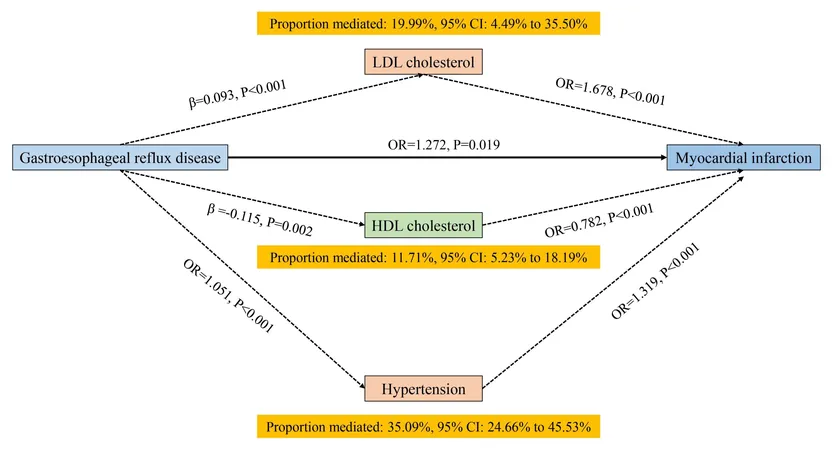
In a surprising twist, the study also unveiled that GERD impacts lipid profiles, showing an association with increased levels of low-density lipoprotein (LDL) cholesterol (β = 0.093, P < 0.001) and triglycerides (β = 0.153, P < 0.001), both notorious for elevating cardiovascular disease risk. Conversely, levels of high-density lipoprotein (HDL) cholesterol, recognized as the "good" cholesterol, were inversely affected (β = -0.115, P = 0.002), further compounding potential heart health issues.
Of particular concern to health professionals is the study's revelation regarding the heightened risk of severe cardiovascular events, such as myocardial infarctions (heart attacks) and hypertension linked to GERD. The odds ratio for a heart attack stood at 1.272 (95% CI: 1.040 to 1.557, P = 0.019), while hypertension was at an alarming 1.357 (95% CI: 1.222 to 1.507, P < 0.001). Interestingly, no significant association was established between GERD and heart failure, indicating that while GERD does pose cardiovascular risks, its effects may vary by condition.
Conclusion
"Our findings suggest that GERD could emerge as a potential risk factor for cardiovascular diseases," asserted Qiang Su. "This study highlights the increasing necessity for early diagnosis and anticipatory strategies addressing both GERD and heart conditions."
With millions globally living with GERD, these revelations could trigger a shift in the approach healthcare providers take toward managing this common disorder. Enhanced awareness of GERD's hidden cardiovascular implications may foster more proactive health strategies, potentially saving lives by uncovering risks that were previously overlooked.
This transformative research not only reshapes our understanding of GERD but also underscores the importance of comprehensive health assessments that consider the interplay between digestive and cardiovascular health. Will this spark a new wave of preventative measures? Stay tuned!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)