Surprising Findings: Anticholinergic Medications Linked to Lower Death Rates But No Increase in Hip Fractures for Parkinson’s Disease Patients!
2024-11-18
Author: Mei
Introduction
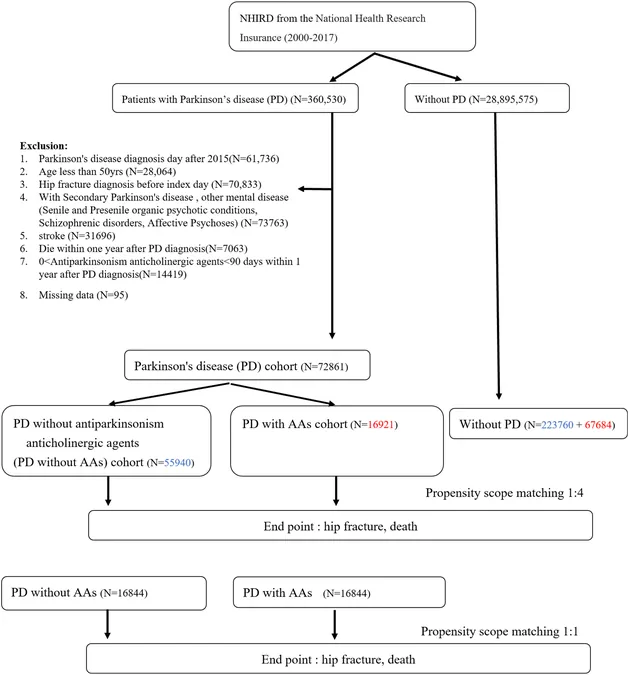
In an intriguing turn of events for the treatment of Parkinson's Disease (PD), a recent study has unveiled that the use of antiparkinsonism anticholinergics (AAs) may not contribute to an increased risk of hip fractures, while being associated with lower mortality rates. This retrospective cohort study relied on data from Taiwan's National Health Insurance Database, marking a significant step in understanding the complex relationship between PD treatments and patient outcomes.
Key Insights from the Study
Researchers analyzed data from patients aged 50 and above, diagnosed with Parkinson’s Disease between January 2000 and December 2015. The study split the participants into three groups: those who had been prescribed AAs for a minimum of 90 days (16,921 patients), those who never had AAs (55,940 patients), and a matched control group of individuals without PD (291,444 patients).
Both PD groups (with and without AAs) exhibited a higher risk of hip fractures compared to the non-PD group, but what’s remarkable is that there was no significant difference in fracture risk between the two PD groups. In terms of mortality, both PD groups significantly surpassed the control group, but the surprising outcome was that those on anticholinergics had a slightly lower mortality, suggesting a complex interaction worth further exploration.
Understanding the Implications
The results indicate that while patients with Parkinson’s Disease are at a higher risk for hip fractures and increased mortality when compared to healthy individuals, the long-term use of anticholinergic medications does not exacerbate these risks. On the contrary, the study showed that the PD patients exposed to AAs experienced a reduction in mortality. This could challenge established perceptions regarding anticholinergics and their safety profile, particularly amid fears surrounding fall-related injuries in PD patients.
The findings are significant given prior studies that have linked anticholinergic medications to an increased risk of fractures in older adults. However, this study positions antiparkinsonism anticholinergics differently, potentially reshaping how physicians view their role in managing PD symptoms such as tremors.
Why This Study Matters
Currently, there’s no consensus in the medical community about the relationship between anticholinergics and hip fracture risks. This research stands out as one of the pioneering studies examining these medications specifically in PD patients, shedding light on their complicated health outcomes. Such insights are crucial for healthcare providers as they make treatment decisions, weighing the benefits of symptom management against the potential risks of medication.
Conclusions and Future Directions
While this expansive study offers a welcome perspective on the use of anticholinergics in Parkinson's Disease treatment, it also indicates a need for further research. Multifactorial influences on PD mortality and the intricate interactions between various medications call for more in-depth studies, particularly those embracing diverse populations and treatment methodologies.
As the medical community seeks to refine treatment guidelines, these insights could lead to more personalized care strategies for PD patients, ultimately enhancing their quality of life. However, the preliminary nature of these results emphasizes a careful approach, advocating for additional, larger-scale studies to validate these findings.
Stay tuned for more updates as we unravel the complexities of Parkinson’s Disease treatment options!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)