Surprising Trends in Candida Species Among HIV Patients in Africa Amidst Universal Test and Treat Policies!
2024-11-27
Author: Li
Introduction
As of 2022, about 38 million people worldwide were living with human immunodeficiency virus (HIV), with an alarming 68% (approximately 25.7 million) residing in Africa. Among individuals living with HIV (PLHIV), conditions like oropharyngeal candidiasis and oral candidiasis are common and serious opportunistic fungal infections that indicate significant immune suppression and can be precursors to acquired immunodeficiency syndrome (AIDS).
Prevalence of Candidiasis in Africa
These candidiasis types can manifest when CD4 T-cell counts drop below 200 cells/μL, impacting about 90% of PLHIV. The prevalence of these conditions varies widely, with reports indicating rates between 4.9% to a staggering 79.4% across African nations. In Africa, where HIV is prevalent and healthcare resources are often scarce, the burden of these fungal infections is severe, leading to difficulties in swallowing, malnutrition, and compromised quality of life.
Rise of Non-Albicans Candida Species
While Candida albicans remains the predominant cause of these infections, responsible for 48% to 87% of cases, the dramatic rise of non-albicans Candida (NAC) species cannot be ignored. Emerging species include C. parapsilosis, C. glabrata, and C. auris, which are increasingly noted for their multidrug resistance, presenting a growing challenge in clinical settings.
Challenges in Management
The management of oral candidiasis often relies on clinical presentations rather than specificity in causative agents, resulting in inadequate treatment options and possible antifungal resistance. The advent of the Universal Test and Treat (UTT) policy in 2015 by the World Health Organization has aimed to enhance health outcomes for PLHIV by promoting immediate antiretroviral therapy (ART) commencement regardless of CD4 count. However, oropharyngeal candidiasis continues to pose significant challenges, especially in resource-scarce settings.
Impact on ART Adherence
One of the most troubling aspects of oropharyngeal candidiasis is its impact on ART adherence. Symptoms such as pain and altered taste sensation can discourage patients from maintaining their treatment regimens, leading to increased risks of drug resistance and complications, including noncommunicable diseases like oral cancer. Furthermore, these infections carry both psychosocial and economic consequences with substantial healthcare costs and diminished productivity.
Importance of Understanding Candida Distribution
Understanding the current distribution of Candida species among PLHIV before and after implementing UTT is crucial for enhancing diagnosis, treatment success, and overall HIV care. This systematic review and meta-analysis aimed to fill that knowledge gap, using rigorous methodologies and statistical analyses to gather data from various studies conducted in Africa.
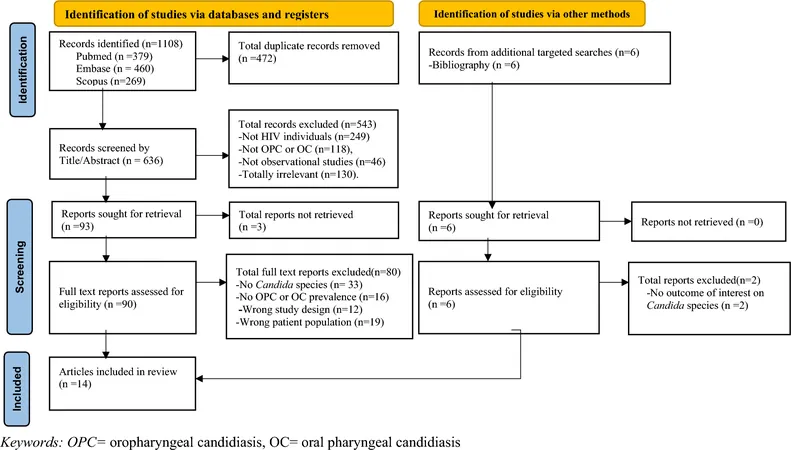
Study Methodology and Results
The search for relevant studies yielded 1108 titles, from which 14 met the criteria for inclusion in the analysis. Among these, C. albicans accounted for 78.7% of isolates, while 19.6% were identified as NAC. The results displayed significant regional discrepancies in prevalence, with Cameroon leading the report with 32.6% of documented isolates, while Uganda had the highest rate of unidentified Candida species.
Conclusions and Recommendations
Critically, the overarching pooled prevalence for oropharyngeal and oral candidiasis among PLHIV was found to be 48%. More significantly, a reduction in oropharyngeal candidiasis from 56% before the UTT policy to 34% afterwards points to improvements potentially linked to the widespread availability of ART.
However, the ongoing presence of NAC species indicates that healthcare systems must step up their diagnostic approaches and patient care strategies. The meta-analysis suggests enhanced laboratory diagnostics and antifungal susceptibility testing to ensure effective treatment for both C. albicans and NAC species.
Healthcare professionals, researchers, and policymakers must leverage these findings to invest in better laboratory practices and research into antifungal resistance, improving outcomes for millions battling HIV and candidiasis across Africa. The implications are clear: insights gleaned from this meta-analysis could very well reshape the future of HIV care in the continent.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)