The Alarming Link Between Metabolic Syndrome and Severe Mental Illness in Ethiopia
2025-04-14
Author: Mei
A Hidden Crisis in Mental Health Care
In a groundbreaking study conducted at Amanuel Mental Specialized Hospital in Addis Ababa, Ethiopia, researchers have unveiled a concerning prevalence of metabolic syndrome (MetS) among patients suffering from severe mental illness (SMI). This alarming intersection of mental and physical health issues raises urgent questions about the overall well-being of this vulnerable population.
Study Insights: What the Numbers Reveal
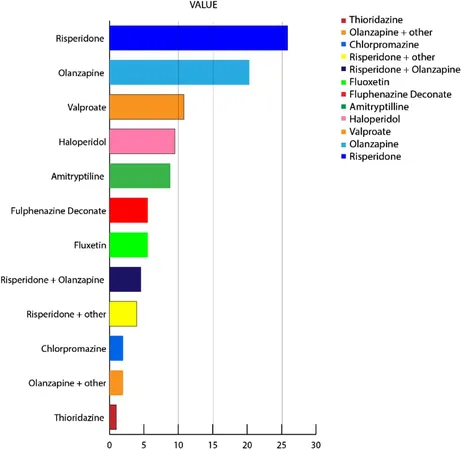
The research, which involved 305 outpatients diagnosed with conditions such as schizophrenia and bipolar disorder, highlights that a staggering 28.5% of these individuals are grappling with MetS. Notably, the prevalence was even higher among schizophrenia patients, reaching 31.5%. The study also found that 88.5% exhibited low levels of high-density lipoprotein (HDL), a critical marker for cardiovascular health.
Risk Factors Uncovered
Several risk factors associated with MetS were identified through rigorous analysis. Age, educational level, length of treatment, and alcohol consumption significantly impacted the odds, with older patients and those holding secondary education or higher being more susceptible to metabolic issues.
The Weight Crisis: Overweight and Obesity Trends
The findings didn't stop there—overweight and obesity were also prevalent: 27.2% of participants were classified as overweight, and 4.6% as obese. Factors such as female gender, prolonged treatment duration, and smoking exacerbated risks of excess weight, indicating a dual burden for those already battling mental health disorders.
A Call for Action: Screening and Education Needed
Given these shocking insights, the study advocates for better health education and proactive screening for MetS and its components among mental health patients in Ethiopia. Ensuring both mental and physical health care standards rise is vital for improving outcomes in this demographics.
Global Context: Ethiopia’s Unique Challenges
Globally, MetS is known to increase the risk of cardiovascular diseases and mortality, especially among those with SMI. With Ethiopia facing unique health care challenges—limited access, socioeconomic hardships—this crisis could have profound implications if not addressed.
Conclusion: A Wake-Up Call for Ethiopia’s Healthcare System
As the study reveals, the intertwining of metabolic syndrome and severe mental illness in Ethiopia calls for immediate and coordinated healthcare responses. With the potential for significantly reduced life expectancy among this population, it's time for Ethiopia to take action—ensuring that mental health treatment is paired with comprehensive physical health monitoring and intervention.
This research underscores a crucial point: treating mental illness is not just about managing psychiatric symptoms; it’s also about safeguarding physical health.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)