The COVID-19 Pandemic's Lasting Impact on Tuberculosis Treatment Adherence: A Deep Dive into South Africa’s Directly Observed Therapy Program
2024-10-14
Author: Wei Ling
Introduction
The COVID-19 pandemic has cast a long shadow over healthcare systems globally, with disastrous repercussions for tuberculosis (TB) treatment efforts, particularly in countries like South Africa where TB is endemic. This article delves into a significant study that scrutinizes the effects of pandemic lockdowns on medication adherence within a TB treatment cohort utilizing directly observed therapy (DOT) techniques.
Study Overview
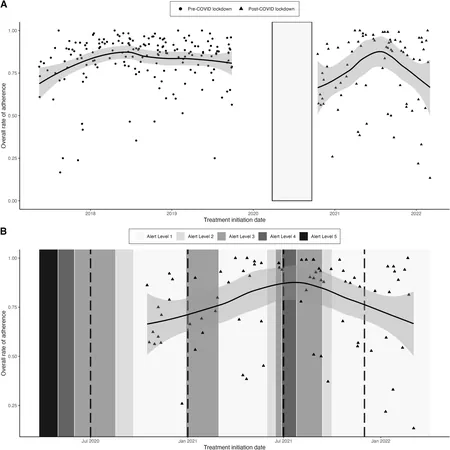
The analysis focused on 263 patients receiving treatment for drug-sensitive TB within the TRUST study framework from May 2017 to March 2022. Participants were divided into two groups based on their enrollment: pre-COVID-19 (before October 2019) and post-COVID-19 lockdown (after September 2020). The study employed sophisticated statistical models, specifically negative binomial regression, to assess and compare non-adherence rates in both cohorts while adjusting for key demographic and behavioral factors.
Key Findings
The results were stark. The TB DOT non-adherence rate increased significantly in the post-COVID-19 group, with a 42% rise (adjusted incident rate ratio of 1.42) compared to pre-lockdown rates, emphasizing the lockdown's disruptive effect on treatment. This trend was most pronounced in the immediate aftermath of the initial lockdown, where the non-adherence rate surged to 74% higher than before.
Such alarming statistics raise challenges regarding continuity of care. From the implementation of strict lockdown measures in March 2020 to subsequent reopenings, key therapeutic interventions were severely curtailed, leading to increased missed doses and decreased patient engagement along with adverse impacts on the healthcare infrastructure dedicated to TB treatment.
Underlying Issues and Broader Context
The research underscores the interplay of COVID-19-induced socio-economic hardships and mental health challenges. Participants underlined significant risks, including high levels of unemployment (73.8% within the post-COVID-19 group) and increased instances of severe underweight status and depression. These factors can drastically impair an individual’s capability to adhere to treatment regimens, highlighting the need for holistic interventions that address both physical and mental health comprehensively.
While the study paints a bleak picture specifically for TB adherence, it reflects a wider global trend observed in countries like India and Iran, where similar lockdown-induced disruptions resulted in rising treatment non-adherence. The world may be grappling with the pandemic’s health ramifications long after immediate restrictions have eased.
Conclusions and Future Directions
The study reveals a critical need to re-evaluate strategies for maintaining TB treatment adherence in post-pandemic settings. With traditional DOT systems impacted, there is an urgent demand for innovative solutions and frameworks that not only restore previous adherence levels but surpass them. Intensive community outreach, psychological support structures, and flexible care models could play vital roles in revitalizing treatment protocols for TB.
In summary, the COVID-19 pandemic has exposed vulnerabilities within TB treatment systems that must be addressed to prevent future escalations in treatment failures and public health crises. The need for continued vigilance and adaptive healthcare responses cannot be overstated—changing the narrative from one of crisis management to one of resilient health systems capable of weathering global challenges.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)