The Critical Journey: Transitioning from Pediatric to Adult Care for Beta-Thalassemia Patients
2024-12-27
Author: Sarah
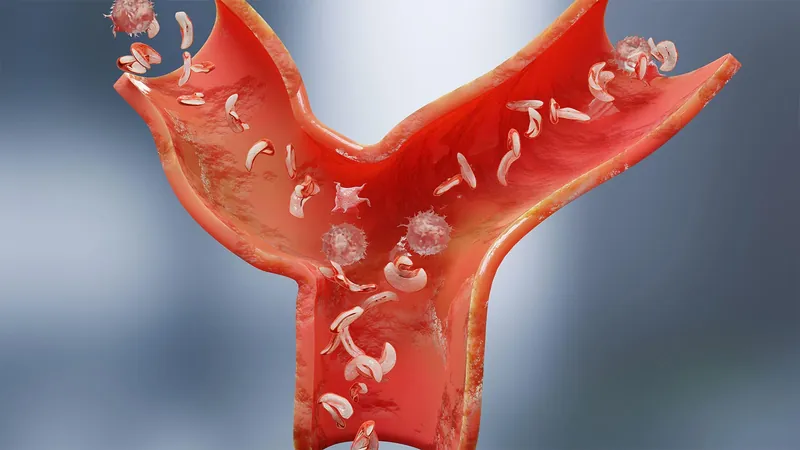
Patients diagnosed with beta-thalassemia major, also known as Cooley's anemia, face a significant health challenge due to a reduction or absence of beta globin in their hemoglobin. This condition leads to severe anemia that necessitates lifelong blood transfusions beginning in early childhood. Despite the harsh realities of this disease that can lead to iron overload and potential organ failure, advances in medical care have transformed the landscape for these patients.
Traditionally viewed as a pediatric condition due to lower life expectancies, the outlook for individuals with beta-thalassemia has markedly improved thanks to routine blood transfusions and enhanced iron chelation therapies. A groundbreaking 2020 review in the European Journal of Haematology highlighted that patients in regions with modern treatment programs now enjoy lifespans comparable to the general population.
Recently, a systematic analysis estimated the global prevalence of thalassemia at an astonishing 1.3 million cases as of 2021, with the highest incidence concentrated in East and Southeast Asia, the Middle East, and the Mediterranean regions. In the U.S., the numbers are projected to be around 4,000—though experts like Dr. Janet Kwiatkowski, Director of the Thalassemia Center at the Children’s Hospital of Philadelphia, argue that this figure might be an underestimate due to increases in immigration and international adoptions.
As more individuals with thalassemia live into adulthood, transitioning from pediatric to adult care becomes increasingly vital. This transition often begins formally around the ages of 12 or 13, focusing on age-appropriate education to ensure patients understand their condition and the necessary care management. Dr. Kwiatkowski emphasizes the importance of transition-readiness checklists that help gauge a young patient’s knowledge about their disease and treatments, which can adapt as they grow older.
Age-Specific Challenges and Complications
Transitions bring unique complications as well. The necessity for regular transfusions and iron chelation remains constant, but the nature of potential health issues evolves with age. Regular monitoring for iron overload in critical organs becomes crucial, utilizing sophisticated techniques like T2* cardiac MRI, which provides detailed assessments of iron deposits in the heart and liver.
Research published in the journal Blood reveals that cardiac issues such as heart failure and arrhythmias can begin manifesting in early adulthood, highlighting the need for vigilant monitoring of these patients. Hepatic complications arising from iron overload, while detectable at any age, tend to present more commonly in adults.
Overcoming Transition Barriers
Dr. Kwiatkowski identifies a significant challenge: the shortage of healthcare providers equipped to manage adult thalassemia patients. Historically, many patients have continued receiving care in pediatric settings due to the lack of experienced adult providers.
A survey encompassing 105 North American patients aged 25 to 44 indicated that approximately one-third remained under pediatric hematologists’ care, largely because those facilities offered more specialized services. In a progressive move, Dr. Kwiatkowski's center collaborates with the Penn Comprehensive Adult Thalassemia Program, ensuring patients receive appropriate adult care that includes advanced imaging and transfusion management.
Looking Ahead: A Call for Specialized Care
The journey for beta-thalassemia patients requires a coordinated effort to establish suitable adult care pathways. As these individuals transition into adulthood, the healthcare system must adapt, overcoming barriers related to provider expertise and logistical challenges to ensure patients can access the specialized care they need. This evolution is not just a matter of transitioning care but also empowering patients to take charge of their health futures.
By focusing on educational initiatives, improving adult care access, and ensuring consistent monitoring for complications, we can better support the thriving community of adults living with beta-thalassemia.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)