The Intriguing Interplay of Technical and Non-Technical Skills in Medical Training: A Comprehensive Overview
2024-12-18
Author: Mei
Introduction
In the realm of medicine, a proficient physician encompasses a diverse skill set crucial for effective patient care. While commonly categorized into technical skills (TS) — such as surgical proficiency — and non-technical skills (NTS) — encompassing vital human factors like communication, decision-making, leadership, and teamwork — the delineation of these skills is being challenged.
Recent research highlights a growing concern over the impact of non-technical skills on medical performance, especially how environmental factors can significantly influence these competencies. This recognition has prompted an increase in training initiatives aimed at enhancing NTS through innovative approaches, most notably simulation-based training. Studies have demonstrated that such training can bolster clinical confidence, knowledge acquisition, and collaboration among healthcare professionals.
Notably, stakeholders in veterinary medicine echo this sentiment, asserting that NTS are equally critical as TS in their field, emphasizing the universal importance of these skills across different medical professions.
Research Findings
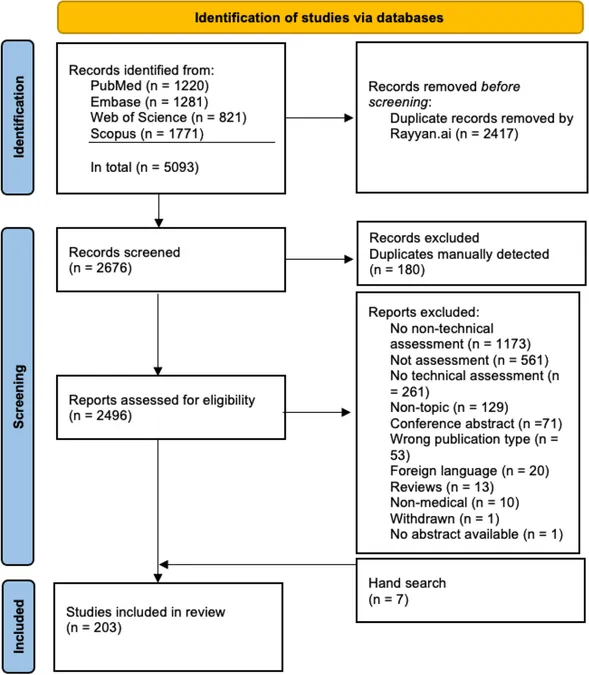
In a recent scoping review, researchers sifted through thousands of studies to examine this multifaceted relationship. Out of over 5,000 initial studies, 203 were rigorously selected for analysis. The findings indicate that 87% of these studies were intervention-based, with the majority employing methods that indicate a positive correlation between TS and NTS.
The correlation studies highlighted critical areas where these skills intersect, particularly in surgical performance, showing that effective teamwork and decision-making enhance technical capabilities. This suggests that a well-rounded training approach incorporating both skill sets could lead to improved patient outcomes.
The Correlation Conundrum
Interestingly, despite a trend where 87% of the studies confirmed a positive correlation, only a fraction of the literature actively tested this interrelation. Such findings raise important questions regarding the methodologies employed in medical education and the clear need for a more integrative approach that systematically assesses both TS and NTS.
The review also encountered significant limitations, primarily stemming from vague definitions of NTS, complicating the assessment and analysis processes. Many studies relied heavily on self-assessment tools, which, while useful, often lack validated backing. The concern persists that subjective assessment may not accurately reflect a learner’s competencies, especially in high-stakes medical environments.
A Call for Future Research
Future investigations must bridge the gap between technical and non-technical skills, promoting a nuanced understanding of how these proficiencies can coalesce to improve clinical practice. By holistically assessing both skill sets, researchers can unlock valuable insights into effective medical education strategies that not only enhance individual performance but ultimately lead to better patient care.
Moreover, the discourse surrounding knowledge as a skill within the NTS framework raises philosophical and educational questions. While knowledge is certainly foundational to any medical practice, its classification as a skill remains contentious.
Conclusion
In a field as dynamic and critical as healthcare, the importance of integrating both technical and non-technical skills cannot be overstated. A clearer, evidence-based delineation of these skills, coupled with rigorous research into their interplay, is essential. This exploration not only stands to enrich medical education but also holds the promise of fostering a more competent and empathetic healthcare workforce.
As we deepen our understanding of these two realms, we must advocate for innovative training methodologies that equip future healthcare leaders with the essential tools to navigate the complexities of patient care in our rapidly evolving medical landscape. The future of medical education depends on it!
Stay tuned for more insights into the world of medical training and the ever-evolving landscape of healthcare competencies. What other hidden connections in medical training could be unveiled?

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)