The Truth About Colonoscopy Screening: Are We Overemphasizing Its Role in Colorectal Cancer Prevention?
2024-11-18
Author: Wei
Background
Colonoscopy has long been hailed as the gold standard for colorectal cancer screening, yet its actual efficacy in preventing the disease remains a topic of fierce debate. The Nordic-European Initiative on Colorectal Cancer (NordICC) trial, the first of its kind to investigate the impact of colonoscopy screening in a randomized setting, revealed no substantial survival advantage for participants who underwent screening compared to those who received usual care. This groundbreaking finding has prompted researchers to revisit the data and challenge the prevailing assumptions about colonoscopy’s benefits.
Methodology
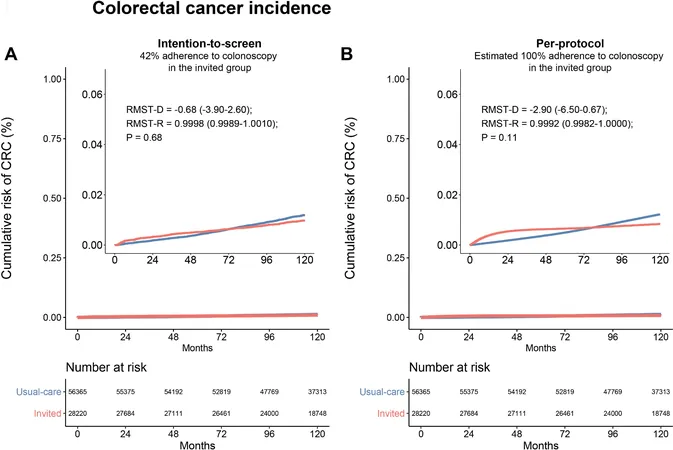
In this reanalysis, which reconstructs individual-level data from the original NordICC trial, experts utilized innovative metrics—Restricted Mean Survival Time Difference (RMST-D) and Restricted Mean Time Loss Ratio (RMTL-R)—to examine cancer incidence and survival outcomes. These measures provide a more robust evaluation compared to traditional methods reliant on hazard ratios, which were deemed unsuitable for the NordICC data due to violations of fundamental assumptions.
Results
The results were telling: for both the intention-to-screen and per-protocol populations, there was no significant difference in the incidence of colorectal cancer over a decade. Participants invited for colonoscopy did not see a measurable reduction in cancer-related deaths. In fact, while those who participated in colonoscopy lived an average of 1.1 days longer cancer-free, this finding did not reach statistical significance.
Conclusions
This comprehensive reanalysis of the NordICC data strongly suggests that inviting individuals for colonoscopy screening does not translate to enhanced survival outcomes compared to routine care. The apparent benefits seen in previous analyses were largely inflated, leading to a questioning of the widespread clinical practice of population-based screening.
The Implications: A Call for Reevaluation
The findings of the NordICC trial and subsequent reanalysis challenge the long-standing belief in colonoscopy as a catch-all solution for colorectal cancer prevention. The study highlighted potential issues in the initial trial design, such as low participation rates—only 42% of those invited actually underwent the procedure—and suggested that many in the usual-care group may have accessed other screening methods that skewed results.
Moreover, colonoscopy's perceived effectiveness must be reconsidered in light of advancements in cancer treatment that have altered survival rates. This nuance suggests that while early detection remains important, the focus should shift towards tailored screening strategies that prioritize high-risk individuals rather than a blanket approach for the general population.
Looking Forward: Precision Medicine in Screening
This pivotal research underscores the necessity of integrating precision medicine into colorectal cancer screening protocols. Individualized risk assessments using data on family history, genetics, and pre-existing conditions may offer a more effective pathway forward. This shift could maximize the benefits of healthcare resources while minimizing the emotional and physical toll associated with unnecessary procedures.
Final Thoughts
As we strive to improve cancer prevention strategies, the reexamination of colonoscopy's role opens the door to more effective, personalized approaches. The entire medical community must engage in this critical dialogue, ensuring that interventions align with actual patient outcomes, rather than tradition or assumption. Time will tell if the colonoscopy screening paradigm will evolve, but the need for rigorous scrutiny of current practices has never been clearer.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)