Uncovering Disparities in Emergency Care for Patients with Substance Use Disorders and Mental Illness: A Nationwide Danish Study
2025-03-31
Author: Jia
Introduction
In an alarming revelation, a recent nationwide study from Denmark has shed light on the quality of emergency care provided to patients suffering from substance use disorders and mental illnesses—conditions that together contribute to a striking increase in morbidity and mortality. This study uniquely evaluates the quality of prehospital and emergency care among three distinct patient populations facing these critical health challenges.
Understanding the Scope of the Study
The researchers analyzed comprehensive data from three major Danish health registries spanning several years: the Danish Prehospital Registry (2016–2017), the Danish Stroke Registry (2010–2018), and the Danish Registry of Emergency Surgery (2008–2018). They aimed to assess prehospital care characteristics and emergency outcomes for patients with mental illness, substance use disorders, and dual diagnoses compared to a control group without these conditions.
Significant Findings on Patient Populations
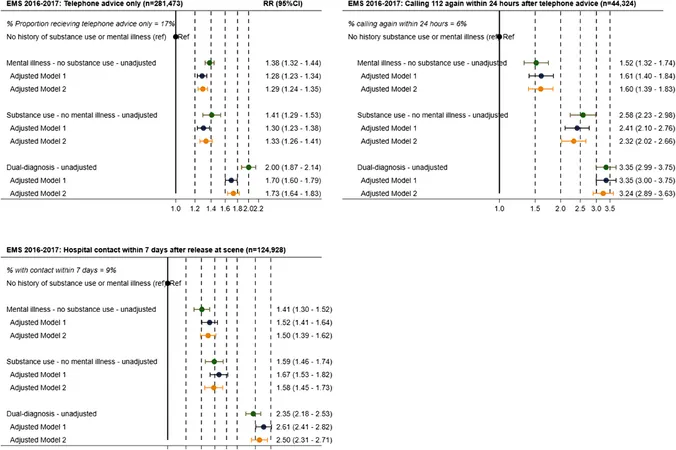
The analysis revealed that out of 492,388 emergency medical service (EMS) calls, approximately 10% involved patients with mental illness, 9% with substance use disorders, and 8% with dual diagnoses. Alarmingly, these patients not only made more repeat calls to EMS within 24 hours but also had higher rates of unplanned hospital visits post-release from EMS—indicating a worrying reliance on emergency services due to unmet healthcare needs.
Strokes and Surgical Delays: A Critical Analysis
The study further assessed patients admitted for ischemic strokes and emergency surgeries for perforated ulcers. Patients with dual diagnoses were less likely to receive life-saving reperfusion therapy compared to their counterparts without mental health or substance use challenges, thereby highlighting inequities in urgent care. The research uncovered that those with mental illness experienced delays in surgical interventions, exacerbating health outcomes and recovery prospects.
The Cost of Inadequate Coordination Between Health Services
The findings underscore a pervasive and troubling reality: the healthcare system often fails to provide integrated treatment for those facing both mental health and substance use challenges. Patients frequently navigate fragmented care pathways that push them towards emergency services rather than more appropriate care options. This gap could potentially lead to longer-term healthcare costs and poorer overall health outcomes.
Proposals for Improvements in Care
To address these disparities, experts recommend implementing integrated care models that unify mental health and substance use treatment approaches. Strategies such as embedding mental health professionals within EMS teams or creating community-based support systems have shown promise. Moreover, specially tailored interventions designed for this high-risk population could significantly improve their emergency care experiences.
Conclusion: A Call to Action
This nationwide Danish study underscores the urgent need for systemic reform in healthcare services to adequately support individuals with mental health and substance use disorders. By elevating the importance of integrated treatment approaches, enhancing training for healthcare providers, and addressing structural barriers within the healthcare system, we can begin to eliminate the disparities that have long plagued these vulnerable patient populations. The implications of this research extend beyond Denmark, as similar healthcare challenges exist globally. As we advance towards an equitable healthcare future, addressing these disparities should be a priority for policymakers and healthcare providers alike.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)