Uncovering the Overlooked: How Multimorbidity and Frailty Skew Kidney Failure Prognostic Models
2024-10-11
Author: Ming
Chronic Kidney Disease (CKD) and Its Rising Prevalence
CKD is on the rise, affecting an alarming 10-15% of adults worldwide. As CKD progresses, it can lead to kidney failure, a serious condition that necessitates kidney replacement therapy (KRT). A multitude of factors contributes to the risk of kidney failure, including age, sex, ethnicity, lifestyle choices, and the management of other health conditions like hypertension and diabetes. But there's more to this story—the presence of other chronic illnesses, known as multimorbidity, and frailty can also critically influence kidney disease progression.
Understanding Multimorbidity and Frailty
Multimorbidity, involving the presence of two or more long-term health issues, is notably common among CKD patients, leading to worse outcomes compared to those without CKD. Frailty, characterized by increased vulnerability and reduced physiological reserve, often accompanies multimorbidity and CKD. Research indicates that these conditions can amplify the risk of hospitalization and mortality in affected individuals.
Interestingly, there's a distinct relationship between multimorbidity and frailty, as some patients experience both, while others may only face one or the other. Current research shows that the measurement of these conditions varies significantly; however, tools such as the Charlson and Elixhauser Comorbidity Indices offer weighted scores that serve to quantify multimorbidity. On the other hand, frailty can be assessed using scales like the Fried Frailty Phenotype or the Clinical Frailty Scale.
The Gaps in Risk Prediction Models
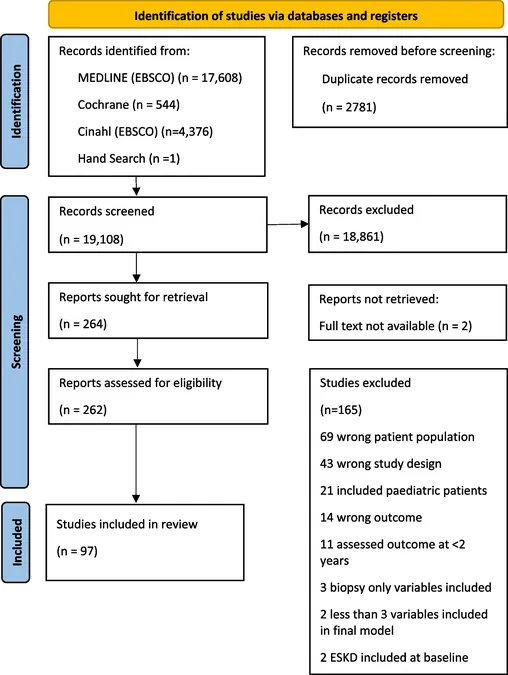
Despite the gravity of multimorbidity and frailty, only a handful of existing risk prediction models take these factors into account. A systematic review covering over 19,000 articles identified just 97 studies meeting the criteria for inclusion, resulting in a total of 121 prognostic models related to kidney failure. Alarmingly, many studies failed to report the prevalence of multimorbidity and frailty among participants, raising questions about the accuracy and applicability of these models.
In fact, among the reviewed studies, a mere handful acknowledged multimorbidity or frailty explicitly. One study showed that individuals facing kidney failure had a higher comorbidity index than those who did not. However, most models, including the frequently validated four-variable Kidney Failure Risk Equation (KFRE), did not account for these crucial conditions, leading to a potential overprediction of risk in frail individuals.
Recommendations for Improved Predictive Accuracy
The findings signal a pressing need for revisiting how risk models are formulated. Current clinical guidelines, such as those from KDIGO and NICE, advocate for using these prognostic models to assist in patient referrals and management decisions. Yet, with the majority of studies lacking a focus on multimorbidity and frailty, we risk making treatment decisions based on incomplete information.
Path Forward: Targeted Research
Future research should aim to include diverse patient populations that accurately reflect those with CKD, multimorbidity, and frailty. Validation calls for recalibrating existing models to enhance their effectiveness in real-world clinical settings. Additionally, it's essential to integrate competing risks into prognostic models, particularly the risk of mortality, which can heavily influence outcomes for patients with multiple health conditions.
Conclusion
In summary, while current risk prediction models provide a framework for anticipating the trajectory of kidney disease, the oversight of multimorbidity and frailty within these frameworks could lead to misguided care strategies. Moving forward, emphasizing these intertwined health aspects will be fundamental to refining prognostic accuracy, thereby ensuring that vulnerable patients receive the individualized care they desperately need.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)