Understanding Trust in Breast Cancer Treatment: Insights from Survivors
2025-01-15
Author: Li
Unique Recruitment Strategy and Participant Profiles
The research team set out to enroll 12 women across two Swiss hospitals, drawing from both German and French-speaking regions. Participants were required to be at least 18 years old, newly diagnosed with breast cancer, and tech-savvy enough to use a tablet for digital diaries. Despite initial hopes to include a diverse group of gynecological cancers, overwhelming challenges meant exclusively recruiting women diagnosed with breast cancer.
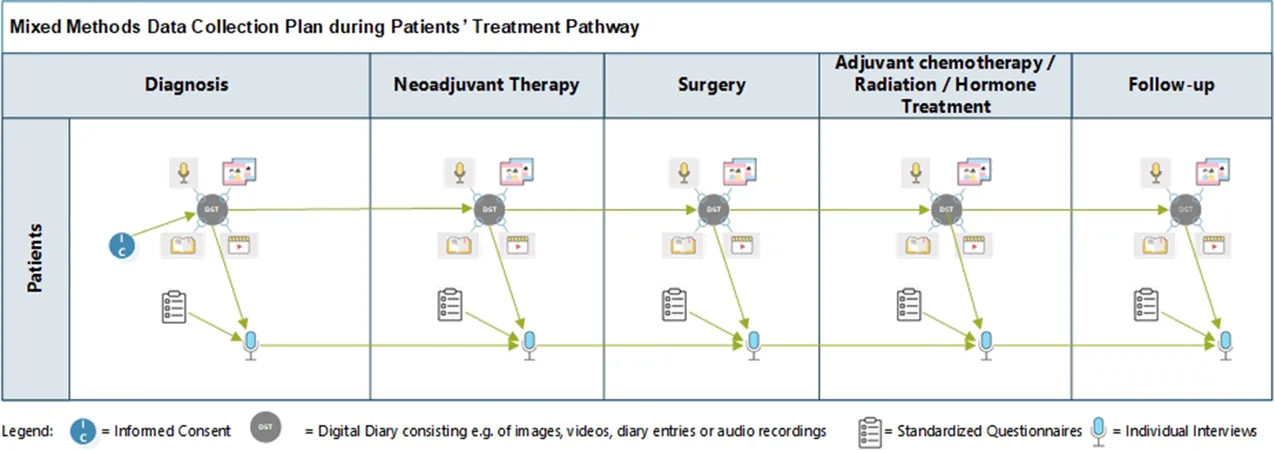
Throughout the study duration from July 2021 to March 2023, participants engaged deeply with their experiences through digital diaries and semi-structured telephone interviews, marking the highs and lows of their treatment journey. Notably, all 12 enrolled women completed the study, revealing strong commitment and engagement with the research.
Digital Diaries: Bridging Emotion and Data
Utilizing the mobile messaging application "Threema," participants recorded their daily experiences in real-time, significantly reducing recall bias. This interactive format facilitated an ongoing dialogue between the participants and the research team, allowing for immediate follow-up on concerns, thus enhancing the richness of qualitative data collected.
Each woman responded to structured surveys at various treatment phases, capturing trust levels towards healthcare professionals and their overall health-related quality of life. Such data indicated a notable trend: a high correlation between trust in medical teams and reported quality of life.
Trust: A Fundamental Element of Care
The concept of trust emerged as a pivotal theme. Quantitative findings reflected a solid trust in healthcare providers, with average trust ratings of 3.7 for physicians and nurses. Yet, experiences varied dramatically; some women reported reduced trust levels tied to specific incidents related to their care. This nuanced understanding of trust was depicted in a comprehensive conceptual model that illustrated how interactions with health professionals shaped their treatment experience.
Participants described the initial encounter with the healthcare system filled with anxiety and uncertainty, particularly during diagnosis. The emotional weight of receiving a cancer diagnosis plunged many into a state of fear and reliance on the perceived competence of their care teams.
Navigating the "Machinery" of Treatment
Women likened their treatment journey to being part of a well-oiled machine, where they alternated between complete trust and feelings of being overwhelmed. Metaphors like a "carousel" and "conveyor belt" highlighted the disorienting yet reassuring nature of structured medical care. For many, consistent interactions with healthcare professionals fostered a sense of security amidst the chaos of treatment protocols.
However, the loss of identity was stark; as one participant poignantly described, the experience of chemotherapy-induced hair loss was a brutal reminder of their new reality as patients. Individual experiences of trust were influenced by personal histories, the healthcare system's competency, and the emotional engagement of nurses and doctors.
The Battle with Mistrust
Conversely, instances of mistrust often arose from contradictory communications among healthcare providers or perceived negligence. Some participants navigated their skepticism by taking an active role in their care, pushing for clarity regarding medications or treatments. Many participants spotlighted the importance of person-centered care characterized by empathy and active listening, which cultivated deeper trust.
The study's findings suggest that nurturing trust in breast cancer care isn’t merely about competence in clinical procedures but also involves addressing the emotional and psychological needs of patients.
Striving for a New Normal
Post-treatment, many women faced continuous challenges re-establishing trust in their bodies and healthcare systems. The fear of recurrence loomed large, overshadowing moments of healing. Yet, the journey revealed a hopeful evolution; women spoke about transitioning toward a new normal—a concept laden with complexity as they reconciled past experiences with their future.
As the study demonstrates, trust in the healthcare relationship critically influences treatment experiences and outcomes. The woven tapestry of women’s voices throughout this research encapsulates the profound impact that trust—or the lack thereof—has on survival, emotional well-being, and life after breast cancer.
Conclusion
This study offers invaluable insights into the intricacies of trust in the breast cancer treatment continuum, highlighting the importance of fostering person-centered care that prioritizes emotional connection alongside clinical expertise. As the healthcare community seeks to enhance the patient experience, these findings are crucial for developing strategies to support women navigating their cancer journeys—a pursuit that may lead to improved quality of life and outcomes across oncology care.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)