Unlocking the Mysteries of Tuberculosis-Related Hemophagocytic Lymphohistiocytosis: A Deep Dive
2024-11-24
Author: Wei
Introduction
Hemophagocytic lymphohistiocytosis (HLH) is a rare and life-threatening syndrome, occurring in approximately 1 out of every 2,000 patients in specialized medical centers. The complexity of diagnosing HLH arises from its diverse symptoms and various trigger factors, which encompass genetic factors, infections, malignancies, and autoimmune diseases. Traditionally, HLH has been categorized into "primary" (genetic) and "secondary" (acquired) forms; however, contemporary classifications delve deeper, highlighting syndromic HLH, disease-specific HLH, HLH mimics, and the Macrophage Activation Syndrome.
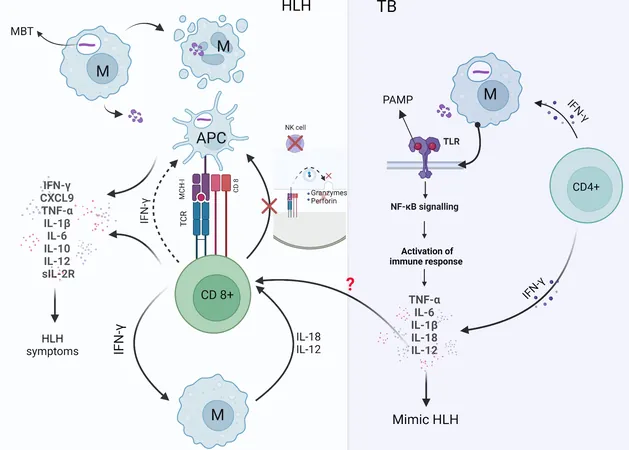
Pathophysiology of HLH and the Role of Tuberculosis
At the heart of HLH's pathophysiology lies a hyperinflammatory response triggered by an overabundance of pro-inflammatory cytokines. Notably, infections—including tuberculosis (TB)—can spark this syndrome. Moreover, disseminated tuberculosis (DTB) often presents similarly to HLH, complicating immune response regulation. On a genetic level, mutations (like PRF1, UNC13D, STX11) are recognized for their role in immune dysfunction, underscoring the intricate interplay between genetic predispositions and environmental triggers.
Infections as Triggers of HLH
Studies indicate that infections account for a significant proportion of HLH cases, particularly among children, where infection-related HLH ranges from 36% to 74%. For adults, infection triggers roughly 50% of HLH cases, and TB alone is responsible for 38% of these infection-related instances. However, these observations stem mostly from literature reports without a robust collection of registry data, suggesting potential biases. This highlights the necessity of thorough investigations into underlying infections, particularly when HLH mimics infectious processes instead of arising from immune dysregulation.
Clinical Presentation and Diagnosis
Clinically, patients with fever, swollen liver and spleen (hepatosplenomegaly), blood clotting issues, low blood counts, and elevated ferritin levels should raise suspicion for HLH. The HLH-2004 criteria, while effective for diagnosing primary HLH in children, often fall short for adult-acquired or secondary HLH cases. Therefore, the H-score was devised as a more suitable tool for adults, incorporating factors that cater specifically to this demographic.
Treatment Strategies
Treatment for HLH necessitates an individualized approach due to the condition's diverse triggers. In stable patients, addressing underlying causes like infections is essential. Conversely, unstable patients may require corticosteroids and intravenous immunoglobulin (IVIG) as frontline therapies. For persistent or difficult cases, emerging regimens (like ruxolitinib or emapalumab) show promise and are becoming part of treatment protocols for HLH.
Tuberculosis Management in HLH Patients
When it comes to tuberculosis, the standard anti-TB regimen includes isoniazid, rifampin, pyrazinamide, and ethambutol (HRZE). Patients with drug-resistant TB or those experiencing adverse reactions may require alternative therapies endorsed by the World Health Organization, further complicating therapeutic choices.
Systematic Review of TB-HLH Cases
Despite the limited patient numbers and lack of diverse language analyses in previous reviews on tuberculosis-associated HLH (TB-HLH), this systematic review seeks to fill this knowledge gap. By analyzing data on TB-HLH globally, we aim to enhance our understanding of demographics, clinical features, lab results, pathology, and treatment outcomes to improve patient management.
Analysis and Findings
Our systematic search initially produced 1,440 records, reducing to 185 studies suitable for in-depth analysis, yielding 213 reports of TB-HLH cases. A majority of the patients (about 61.6%) were male, with a predominant number hailing from India, the United States, and countries with notable immigrant populations, further illustrating the geographical spread of this syndrome. A striking feature of this analysis is the recognition of past infections and comorbidities such as HIV, autoimmune diseases, and malignancies, which can increase susceptibility to HLH.
Mortality and Survival Rates
Notably, the mortality rate for TB-HLH cases stands at approximately 39%, with higher rates observed among older patients, those with specific comorbidities, and individuals with low platelet counts or elevated LDH levels. Furthermore, treatment approaches revealing higher survival rates—including combined therapy with ATT and HLH-specific treatment—underscore the importance of comprehensive management strategies tailored to patient needs.
Conclusion
In conclusion, our research highlights vital insights into the diagnosis, epidemiology, and treatment of TB-HLH, revealing the critical role of both anti-TB treatments and immunomodulatory therapies like IVIG. As the understanding of this complex condition evolves, it is crucial for healthcare providers to maintain heightened vigilance for HLH, especially in patients displaying classic symptoms like fever and hepatosplenomegaly, particularly those with prior TB exposure. The ongoing need for research into preventative strategies and the exploration of treatment combinations remains paramount in improving outcomes for these patients.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)