Unlocking the Potential of Vitamin D: A Game-Changer in Managing Obesity and Hyperandrogenism in PCOS Models!
2024-11-09
Author: Yu
Recent Research
Recent research has shed light on the promising therapeutic effects of Vitamin D in combatting obesity and hyperandrogenism associated with Polycystic Ovary Syndrome (PCOS) in a mouse model. This groundbreaking study, approved by the Ethics Committee of Fujian Maternity and Child Health Hospital, sought to explore the impact of Vitamin D on female mice subject to conditions mimicking PCOS through a combination of low-dose DHEA and a high-fat diet.
Experimental Setup and Findings
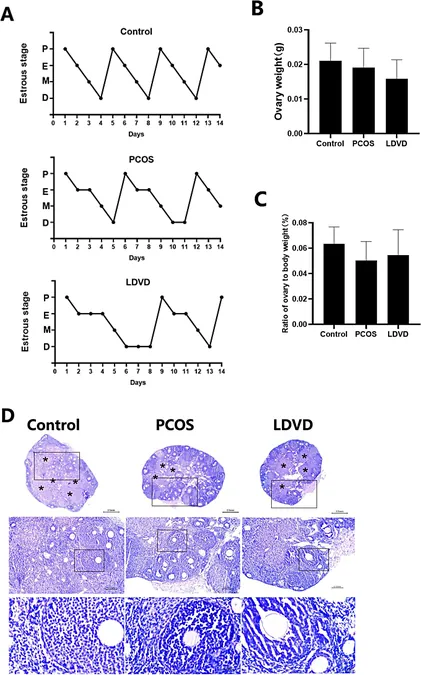
Female mice, aged 21 days, were meticulously housed in a controlled environment and divided into four distinct groups: control, PCOS, PCOS with low-dose Vitamin D (LDVD), and PCOS with high-dose Vitamin D (HDVD), with ten mice per group. The PCOS model was induced using a high-fat diet—comprising 60% fats along with DHEA injections—aimed at replicating the metabolic and reproductive anomalies commonly seen in women with PCOS.
After administering Vitamin D via intraperitoneal injection over 40 consecutive days, researchers identified significant differences across groups. The control group displayed normal estrous cyclicity, while the PCOS groups exhibited disrupted cycles. Notably, while both the LDVD and HDVD groups presented abnormal estrous cycles, the LDVD group showed a reduction in body weight compared to the increased weight in the PCOS group. Astonishingly, the HDVD group experienced severe adverse effects, eventually leading to mortality, shedding light on the potential toxicity of excessive Vitamin D.
Impact on Serum Biochemical Markers
Further analysis revealed that the serum 25-hydroxyvitamin D (25(OH)D) levels were notably higher in the LDVD group, underscoring the effectiveness of Vitamin D supplementation. Simultaneously, hormone levels indicated that testosterone concentrations were drastically elevated in the PCOS group, while Vitamin D administration successfully reduced hyperandrogenism, bringing testosterone levels closer to that of the control group.
Liver health was also compromised in the PCOS group, exhibiting signs of steatosis, whereas the LDVD group showed improvement, although caution was warranted due to the undesirable effects seen in the HDVD group. Such improvements align with other research indicating that Vitamin D can mitigate liver damage and fat accumulation in various metabolic conditions.
Broader Implications for PCOS and Obesity Management
The implications of these findings extend beyond animal studies. PCOS, a leading cause of anovulatory infertility among women, is often linked with obesity—an epidemic that exacerbates health complications globally. Current treatments such as bariatric surgery are invasive and carry risks, hence Vitamin D might provide a critical, non-invasive alternative worth exploring.
Despite prior inconsistent results regarding the efficacy of Vitamin D in weight management, this study shines a light on the need to re-evaluate the potential of Vitamin D in treating obesity-related issues, particularly in women with PCOS. Given that Vitamin D deficiency correlates with obesity in the broader population, further research into optimal dosages and methods of administration is paramount.
Limitations and Future Directions
The current study, while illuminating, does have limitations, including the lack of certain hormonal assessments and a focus primarily on animal models. It calls for future investigations to explore the underlying mechanisms driving these therapeutic effects and to transition toward clinical trials to validate these promising results in human subjects.
Conclusion
In conclusion, Vitamin D is proving to be a possible cornerstone in addressing the complex interplay between PCOS, obesity, and hyperandrogenism. It raises an exciting possibility that simple supplementation could help unlock a healthier future for many women battling these challenges—stay tuned for further developments on this revolutionary front!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)