
Unlocking the Secrets of Vulvovaginal Biopsies: Essential Insights from a Leading Dermatologist
2024-11-17
Author: Sarah
In an eye-opening session at the 2024 Society of Dermatology Physician Associates (SDPA) Fall Conference in Las Vegas, Dr. Audrey Rutherford, a board-certified dermatologist from the Dermatology and Aesthetics Center of Utah, shared crucial insights regarding the underdiagnosed realm of vulvovaginal skin conditions. Highlighting the critical nature of these assessments, she firmly stated, “If you are ever concerned about cancer, just biopsy." Her message underscores the importance of vigilance in identifying potential malignancies, particularly when it comes to conditions affecting women's vulvas.
Dr. Rutherford’s session tackled the often overlooked field of vulvovaginal dermatology, pointing out that many women do not routinely examine their vulvas, and gynecologists may lack the dermatological training necessary for comprehensive care. Thus, the prevalence of vulvar skin disorders can frequently go unnoticed, leading to delayed diagnoses.
When Should You Biopsy? A Cancer-First Approach
Dr. Rutherford emphasized the critical factors that warrant a biopsy. One of her foremost recommendations is to prioritize cancer concerns when evaluating vulvar lesions. Indicators of potential vulvar cancer that warrant a biopsy include areas that appear like the “ugly duckling,” non-healing spots, treatment-resistant lesions, and any signs of skin hardening.
However, she reassured attendees that not all non-cancer diagnoses require a biopsy. There are numerous non-cancerous conditions that may justify obtaining a sample, such as uncertain diagnoses, skin that does not respond to treatments, and atypical presentations involving changes in color, texture, or blistering.
Best Practices for Biopsy Procedures
When performing biopsies, Dr. Rutherford presented two ideal techniques: the punch biopsy and suture-assisted biopsy. Punch biopsies are particularly useful for assessing depth in conditions like squamous cell carcinoma, while suture-assisted biopsies are adaptable for most non-cancer concerns.
Key tips from her practice include:
1. **Avoid biopsying the midline** (including the clitoris, urethra, and anus).
2. **Biopsy distinct areas** that show different morphological characteristics.
3. **Utilize topical numbing cream** beforehand, noting that the effectiveness can vary between hair-bearing and non-hair-bearing regions.
4. **Post-care recommendations include using Vaseline and pads**, steering clear of traditional bandages.
Moreover, Rutherford stressed the importance of detailed pathology communication. Providing pathologists with comprehensive information about lesion characteristics, previous treatments, and the clinician’s concerns can lead to quicker and more accurate diagnoses.
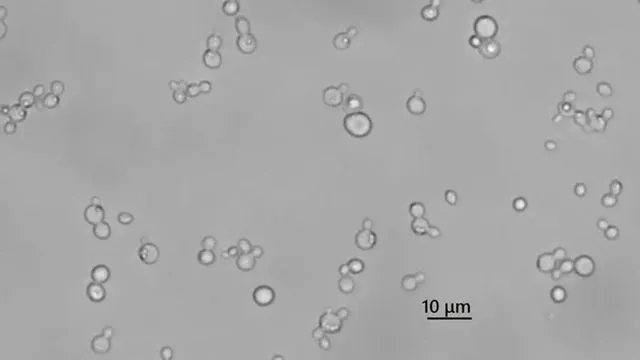
Understanding the Biopsy Process: The 2mm Consideration
Another crucial point Dr. Rutherford made is related to the difference in measurement between 2mm on the skin's surface versus what is needed histologically. While minor variances in size may not affect healing, they can significantly impact diagnostic clarity. She advised practitioners to avoid samples smaller than 3mm to enhance the chances of accurate pathology results.
Final Takeaways
The overarching message from Dr. Rutherford’s session was unequivocal: when cancer is a potential issue, biopsies should not be overlooked. Clinicians must harmonize patient care with the need for precise diagnostics, ensuring that large enough samples are taken to facilitate thorough investigations. While the prospect of biopsies may be daunting, their role in clarifying unclear diagnoses and guiding treatment cannot be overstated.
As specialists in the field further their understanding of vulvovaginal dermatology and empower patients with knowledge, the hope is that outcomes will improve, and underdiagnosed conditions will become a thing of the past. Don’t let fear dictate your practice; advocate for women’s health by making those biopsies when it counts!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)