Unlocking the Secrets to HIV Partner Status Notification: What We Discovered About Barriers and Solutions in Low-Income Countries
2024-12-18
Author: Arjun
Unlocking the Secrets to HIV Partner Status Notification: What We Discovered About Barriers and Solutions in Low-Income Countries
In a bold bid to end the HIV pandemic, UNAIDS has set the daunting 95-95-95 targets to hit by 2030. This ambitious strategy aims to diagnose 95% of all individuals living with HIV, get 95% of those diagnosed on antiretroviral therapy, and achieve viral suppression in 95% of those undergoing treatment. Despite substantial progress—where, as of 2019, 81% of people worldwide were aware of their HIV status—the journey remains fraught with challenges. Approximately 82% of those diagnosed were on antiretroviral therapy, and about 88% of those achieved viral suppression. However, only 59% of the total population living with HIV worldwide are virally suppressed.
To effectively reach the 95-95-95 targets, an innovative solution lies in encouraging individuals to disclose their HIV status to their partners, tapping into the powerful role that partner status notification plays in identifying those undiagnosed while increasing testing procedures. Since 2012, the WHO has recognized this mechanism as vital to HIV testing services. Partner status notification not only enhances testing rates but also diminishes risky behaviors associated with HIV transmission.
Yet, there are concerning disparities when it comes to the experience of women living with HIV—53% of the global HIV population—who face unique hurdles in notifying their sexual partners due to social stigma, gender inequality, and economic dependence. Earlier studies in high-income regions identified supportive relationships and community connection as facilitators for effective partner notification, but these vary largely in lower-income countries where socio-cultural dynamics play a critical role.
Low- and lower-middle-income countries are disproportionately affected by HIV, facing barriers stemming from structural inefficiencies, cultural biases, and limited resources. These regions grapple with distinct HIV epidemics marked by varying levels of severity and risk behaviors, complicating efforts to implement comprehensive healthcare responses.
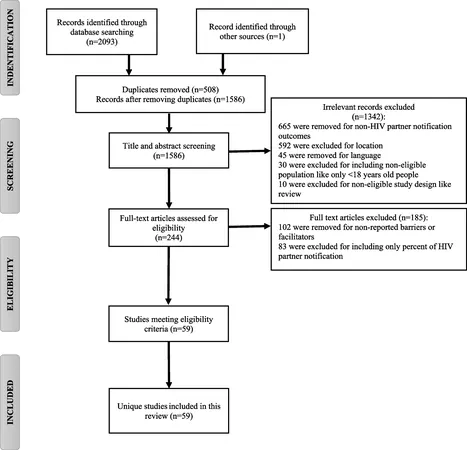
A systematic review has sprung forth to delve into the barriers and facilitators of HIV partner status notification particularly within these resource-constrained regions. It emphasizes the essential need for strategies that can empower individuals without increasing their risks—an ongoing conundrum.
Significant findings highlight pervasive fears of stigma and discrimination as major barriers preventing open conversations about HIV status. Many individuals also fear violence, abandonment, and loss of financial support if they disclose their status. Factors such as multiple partners and lack of information on how to approach the notification process create additional challenges. Conversely, supportive partner relationships, cultural shifts toward increased HIV literacy, and open communication have emerged as facilitators that can help mitigate these risks.
The insistence of health professionals on integrating partner notification services within HIV testing frameworks remains paramount, yet barriers persist, especially among vulnerable populations like queer communities and sex workers.
Strategies that incorporate innovative methods like HIV self-testing and community engagement prove potentially transformative, although the uptake faces challenges such as financial costs and user mistakes. Furthermore, discussions surrounding the concept of "undetectable equals untransmittable" (U=U) remain conspicuously absent from patient-provider dialogues, despite its critical importance in contextualizing risks and encouraging safer practices.
Finally, as we look to the future, it is clear that comprehensive approaches tailored to specific cultural, geographic, and economic contexts, combined with community involvement and innovative healthcare tactics, stand as our best hope in improving partner status notification and, ultimately, reducing the HIV epidemic.
As we work toward realizing the 95-95-95 vision, the imperative becomes clear: stigma must be obliterated, and support must be amplified, ensuring that no one has to navigate their HIV journey alone. How can we catalyze change in these areas? What innovative solutions can reshape this narrative? The answers lie in collective advocacy, informed healthcare practices, and a society unafraid to talk about the realities of HIV.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)