Unmasking a Hidden FSH-Secreting Pituitary Adenoma: A Surprising Discovery After Ovarian Hyperstimulation Syndrome
2024-12-21
Author: Daniel
Understanding Ovarian Hyperstimulation Syndrome (OHSS)
Typically arising from infertility treatments, Ovarian Hyperstimulation Syndrome (OHSS) is characterized by the "spoke-wheel" appearance of the ovaries—bilaterally enlarged and studded with cysts of varying sizes. While most cases are triggered by medications like human menopausal gonadotropin (HMG) and human chorionic gonadotropin (hCG), OHSS can also manifest due to elevated hormone levels from tumors, including follicle-stimulating hormone (FSH) and hCG. Nevertheless, misinterpretations of serum FSH levels can lead to significant clinical pitfalls.
A Case Study that Baffled Experts
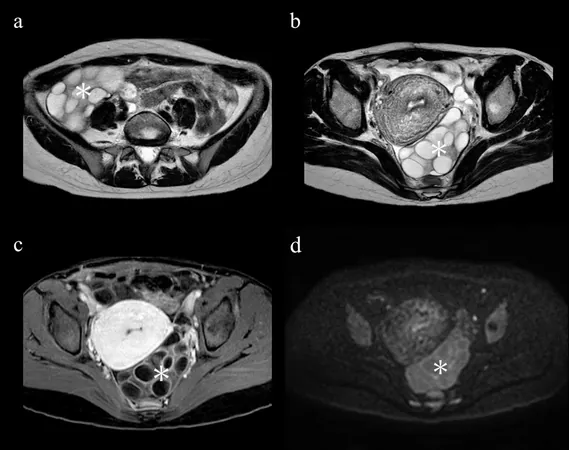
Meet a 29-year-old Japanese woman with no prior pregnancies who came seeking help for irregular menstruation while hoping for fertility treatment. During her initial assessment, ultrasound revealed bilateral ovarian masses, prompting referral to our specialized hospital. An MRI suggested classic signs of OHSS, leading to tests for hormone levels including FSH and hCG.
Elevated estradiol levels (737 pg/ml), but normal FSH and hCG readings, initially indicated that estrogen was the likely culprit behind the uterine dysfunction. These findings led her doctors to suspect estrogen-producing ovarian tumors and schedule her for surgical intervention.
However, further examination using CT scans revealed an unexpected pituitary lesion, ultimately diagnosed as an FSH-secreting pituitary adenoma. The groundbreaking revelation meant that the scheduled ovarian surgery could be avoided, and she could instead be treated for the actual source of her symptoms.
Insights and Implications from the Case
This case underscores a crucial lesson for clinicians: even when serum FSH levels appear normal, the possibility of an FSH-producing pituitary adenoma should not be dismissed. Elevated estrogen confounds diagnosis, affecting FSH and LH levels due to feedback mechanisms. It took a worrying four months for healthcare providers to identify the FSH-secreting adenoma, and misinterpretation of hormone levels could have led to unnecessary surgical intervention.
A comprehensive review of the literature reveals that FSH-producing tumors account for less than 1% of all pituitary adenomas, adding to the rarity and complexity of such cases. Clinicians must maintain a high index of suspicion for these tumors, particularly when encountering atypical presentations of OHSS.
Post-Surgery Recovery and Next Steps
After surgical removal of the adenoma, the patient's hormone levels normalized over the following months, leading to a resumption of regular menstrual cycles. Despite subsequent fertility treatments, including intracytoplasmic sperm injection, the patient has yet to achieve pregnancy, highlighting the ongoing challenges faced by many couples struggling with infertility.
Conclusion: A Cautionary Tale for Medical Professionals
This striking case serves as a vital reminder for healthcare providers about the potential pitfalls in diagnosing ovarian conditions amidst complex hormonal landscapes. Prompt and accurate interpretation of hormone levels, informed by detailed imaging studies, can be critical in avoiding unnecessary treatments and ensuring appropriate patient care. As OHSS linked to FSH-secreting tumors remains a rare yet significant challenge, vigilance in diagnosis and consideration of atypical hormonal presentations is essential for achieving optimal patient outcomes.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)