Unmasking Influenza: Tracking Virus Trends in Northeast Italy from 2017 to 2024
2025-04-24
Author: Sarah
A Deep Dive into Flu Seasons
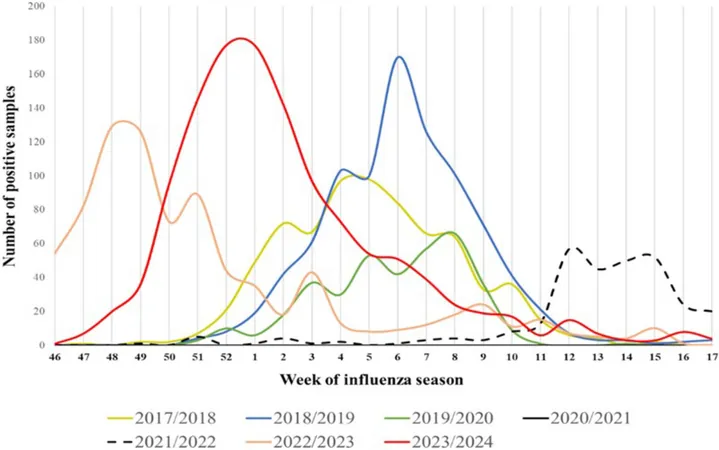
From the 2017/2018 to the 2023/2024 flu seasons, a staggering 21,180 respiratory samples were analyzed in the Veneto region of Northeast Italy, revealing critical patterns in influenza circulation. The season that saw the most action was 2023/2024, with 6,718 samples collected, while the pandemic years of 2020/2021 and 2021/2022 saw a significant drop in testing.
Overall, 4,325 samples tested positive for influenza, accounting for 20.42% of all tested cases. The positivity rates fluctuated dramatically, with a low of 14.86% in 2019/2020 and skyrocketing to 34.55% during the predominantly unaffected 2021/2022 season.
The Pandemic's Impact
No influenza cases emerged during the height of the COVID-19 pandemic in 2020/2021, a stark contrast to the active years preceding and following it. After a return to normalcy in the 2022/2023 season, there was renewed activity, showcasing how influenza could bounce back with vengeance post-pandemic.
Influenza Virus Breakdown
Among the positive samples, Influenza A viruses (IAVs) dominated, making up 78.68% of cases, particularly during the pre-pandemic seasons. Interestingly, Influenza B viruses (IBVs) accounted for at least 10% in most seasons, with the highest prevalence noted in 2017/2018 where they accounted for over 70% of samples.
Analyzing Seasonal Patterns
Each flu season typically peaked between weeks 5 and 6. However, the unusual dip in testing during the COVID-19 pandemic challenges previous patterns. The data from the influenza seasons indicates a shift in dominant strains, with the A(H1N1)pdm09 subtype making a noticeable comeback in the recent season.
Age Dynamics and Influenza Medical Concerns
Analyses reveal that adults, particularly those aged 65 and older, experienced significant influenza circulation. In stark contrast, a shift occurred in 2021/2022, where the majority of reported cases were from the 15-44 age group, likely influenced by pandemic vaccination strategies.
The impact of influenza extends well beyond seasonal woes; it poses substantial public health risks, particularly in vulnerable populations aged 65 and above. Despite the existence of vaccines, widespread vaccine hesitancy stands as a significant barrier to effective prevention.
The Power of Surveillance
To implement effective control strategies, robust surveillance systems and lab capacities are essential. Italy’s RespiVirNet provides crucial data to refine diagnostic and intervention strategies, improving the health system's preparedness against potential flu pandemics.
The Road Ahead: Vaccination and Viral Trends
The data illustrates a growing concern surrounding the efficacy of vaccines against evolving strains. The dominant circulation of A(H3N2) in prior years has seemingly fortified immunity against it, creating vulnerability to A(H1N1)pdm09. With low vaccination rates reported across age groups, particularly under 60, public health campaigns are vital.
As we advance towards late 2023 and beyond, the resilient nature of influenza viruses requires adaptive strategies and sustained vigilance to safeguard public health and manage potential future outbreaks.
Final Thoughts
As researchers delve deeper into the challenges presented by influenza and its variants, ongoing monitoring and adaptive strategies will be critical to mitigating risks associated with this ever-evolving virus.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)