Unmasking the Hidden Crisis: Postpartum Sepsis in Urban Karachi and How We Can Combat It
2025-04-16
Author: Rajesh
Understanding Postpartum Sepsis: A Global Health Threat
Postpartum (PP) sepsis is a critical infection of the genital tract and is alarmingly the third leading cause of maternal mortality globally. Defined as occurring within 42 days after childbirth, this life-threatening condition can lead to severe complications for both mothers and their newborns. Recent studies reveal a staggering 21 million new cases of maternal sepsis annually, leading to 17,000 deaths around the world. Alarmingly, approximately 11% of maternal deaths are attributed to postpartum sepsis, particularly rampant in middle and low-income countries.
Pakistan's Grim Reality: A Spotlight on Maternal Mortality
In Pakistan—a lower-middle-income country with inadequate health infrastructure—the maternal mortality rate stands at 186 deaths per 100,000 live births. A shocking 96% of these deaths are attributed directly to obstetric complications, with PP sepsis ranking as the third leading cause. The situation worsens in rural areas where 28-42% of births occur at home, often attended by unskilled birth attendants, complicating data collection and increasing risks.
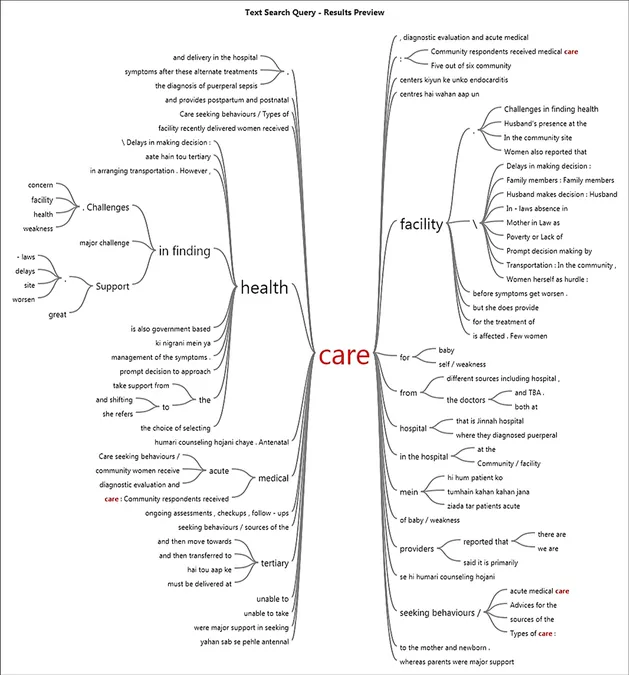
The Cultural and Social Barriers to Care-seeking
Despite existing national guidelines for sepsis management, timely identification and intervention for postpartum sepsis remain critical challenges. Using the "Three Delays" model of maternal mortality, it becomes evident that delays in care-seeking, reaching healthcare facilities, and initiating treatment are key factors leading to increased mortality. Cultural beliefs, limited maternal health knowledge, and the dominance of traditional healing practices often delay necessary medical intervention.
Unveiling Care-seeking Behaviors in Karachi
Conducted in semi-urban Karachi, a recent study explored the care-seeking patterns of women suffering from PP sepsis through 32 in-depth interviews. The study highlighted that women often prefer alternative care sources such as traditional birth attendants, spiritual healers, and unlicensed chemists over recognized health facilities. Surprisingly, many women lacked knowledge of PP sepsis symptoms, mistaking them for normal postpartum issues, thereby delaying critical treatment.
Real-Life Stories: The Impact of Misguided Care Choices
One participant’s story illustrates the dire consequences of seeking alternative care. After experiencing severe postpartum symptoms but initially relying on faith healing, the woman eventually deteriorated and had to be admitted to a hospital, underscoring the necessity of early medical intervention. Financial constraints frequently dictate healthcare decisions, pushing families to opt for less reliable treatment sources.
Urgent Calls for Community-Based Interventions
To combat postpartum sepsis effectively, initiatives must focus on community education, targeted campaigns promoting awareness of symptoms, and systematic training for local health workers. Engaging family members, particularly male household heads, is crucial to ensure that women receive the support needed to seek prompt care during the postpartum period. Strengthening local healthcare infrastructure to adequately handle obstetric emergencies is another imperative step towards reducing morbidity and mortality.
A Path to Improvement: What Needs to Change
To reduce the prevalence of postpartum sepsis and its associated mortality, systemic changes are essential. These include enhancing education around maternal health, improving healthcare accessibility, and extending affordability of services. Ultimately, a collaborative approach engaging community health workers, local stakeholders, and healthcare facilities will pave the way for timely interventions and better outcomes for maternal health in Pakistan.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)