Unraveling the Complex Relationship Between Frailty and Acute Respiratory Distress Syndrome: Insights from a Mendelian Randomization Study
2024-11-29
Author: Arjun
Recent research has illuminated the intricate relationship between frailty and Acute Respiratory Distress Syndrome (ARDS), a condition that poses a significant risk for critically ill patients. Frailty is a state of increased vulnerability resulting from multiple organ system deterioration, and it affects over 40% of older adults in long-term care. Observational studies have drawn connections between frailty and increased severity of chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), as well as heightened mortality rates in critically ill patients. However, the debate surrounding the interplay between frailty and ARDS has continued, urging for more conclusive findings.
ARDS is a severe and often fatal condition precipitated by various factors, most notably pneumonia and non-pulmonary sepsis. Alarmingly, it contributes to 10% of Intensive Care Unit (ICU) admissions, with mortality rates soaring to as high as 45%, particularly among patients requiring mechanical ventilation. Studies have indicated a correlation between frailty and ARDS; a noteworthy investigation of over 3,000 individuals found that frailty significantly increased the risk of respiratory impairment. Other research demonstrates that frailty is linked to adverse prognostic outcomes among ARDS patients, particularly those experiencing viral pneumonitis. Yet, conflicting evidence from a longitudinal study found no substantial relationship between prehospital frailty and ARDS development, sparking crucial questions about the nature of these associations.
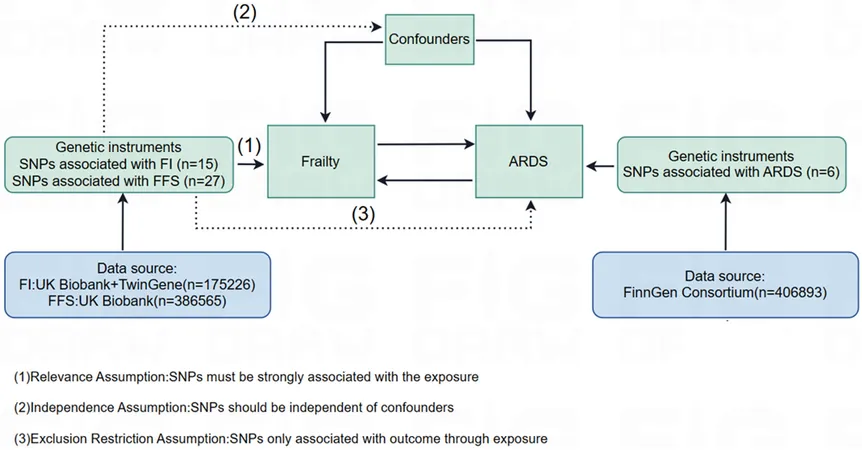
To further examine these relationships, a recent study turned to Mendelian Randomization (MR) - a statistical approach that helps clarify causal links between risk factors and clinical outcomes while reducing confounding biases. Utilizing genome-wide association studies (GWAS), researchers conducted a bidirectional analysis to explore the causal interplay between frailty and ARDS. The findings, however, brought light to the complexity of these relationships. Despite applying various statistical techniques and ensuring robust instrument selection, the analysis revealed no significant causal relationship between frailty and ARDS.
Interestingly, when analyzing common risk factors associated with both conditions, phenomena such as body mass index (BMI) and cognitive performance emerged as noteworthy influencers. Higher BMI was linked to a 2.3 times increased risk of ARDS, while improved cognitive functioning correlated with lower ARDS risk. These insights raise vital considerations for clinical practice, suggesting that while frailty may not induce ARDS, assessing a patient’s frailty could guide rehabilitation strategies in ARDS recovery.
Despite no direct evidence supporting the link between frailty and ARDS, the nuances of the findings emphasize the need for clinicians to recognize that ARDS can develop in seemingly low-risk populations, including younger individuals without prior frailty histories. Therefore, while frailty assessments shouldn't dictate clinical decisions or ICU admissions, they remain crucial components in providing tailored post-recovery care.
Importantly, the study faced several limitations, such as a small sample size for ARDS analysis and focus on a homogenous population, which can limit the applicability of results across diverse demographic groups. Future research efforts should not only seek to confirm these findings but also delve deeper into subtype-specific interactions of frailty and ARDS to unlock advanced understanding and targeted interventions for both conditions.
In summary, while this study failed to establish a direct causal relationship between frailty and ARDS, the implications of its findings are significant, urging a reevaluation of how we perceive and manage these conditions in critically ill patients. As the medical community continues to uncover the complexities surrounding frailty and ARDS, the quest for knowledge remains crucial in enhancing patient care and outcomes.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)