Unraveling the Hidden Role of Neutrophils in Severe COVID-19: A Game-Changer for Treatment
2024-12-18
Author: Rajesh
Introduction
As the world tackled the COVID-19 pandemic, researchers identified a troubling pattern: patients with high levels of neutrophils, the body's frontline immune defenders, often faced severe illness and deteriorating health outcomes. But what was the underlying mechanism driving this alarming trend? A groundbreaking study from Trinity College sheds new light on this crucial aspect of COVID-19 pathology, potentially revolutionizing treatment strategies for the most severely affected patients.
The Role of Neutrophils in COVID-19 Pathology
Published in the prestigious journal JCI Insight, this study reveals the significant—yet often overlooked—role of neutrophils in battling COVID-19. Historically, these abundant immune cells have been somewhat neglected in research, primarily due to challenges in studying their dynamic functions. However, advances in immunology are exposing their pivotal roles in various diseases, including viral infections, cancers, and autoimmune conditions.
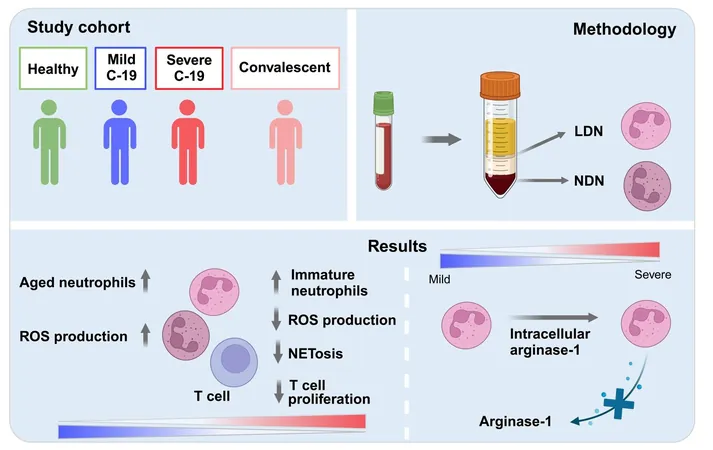
Dysfunction of Neutrophils in Severe Cases
In numerous cases of COVID-19, neutrophils can become dysfunctional, transforming a manageable infection into a critical threat to life. Understanding the mechanics behind neutrophil behavior in the context of COVID-19 severity is crucial. The research team found that severe COVID-19 patients exhibit heightened levels of low-density neutrophils (LDNs), a dysfunctional subset of neutrophils. Remarkably, neutrophils from severe cases displayed immature characteristics and a dysfunctional response compared to their counterparts in mild cases.
Key Discoveries Regarding Neutrophil Functionality
One of the study's standout discoveries is the impairment in neutrophils’ ability to produce critical immune components, such as neutrophil extracellular traps (NETs) and reactive oxygen species (ROS), both vital for combating SARS-CoV-2, the virus responsible for COVID-19. Encouragingly, researchers noted an unexpected failure in neutrophils from severe cases to secrete arginase-1—an enzyme typically released to temper inflammation—despite elevated intracellular levels. This unexpected malfunction could exacerbate inflammatory responses, perpetuating immune dysfunction even after recovery, raising questions about long-term health repercussions.
Expert Insights
According to Dr. Conor Finlay, senior research fellow at the School of Medicine, “Our research indicates that the neutrophil, often seen as merely a participant in immune defense, is intricately linked to the severity of COVID-19.”
Implications for Treatment
Adding to the complexity, the study indicates that conventional treatments like dexamethasone—an anti-inflammatory agent frequently utilized for severe COVID-19—may further complicate neutrophil functionality. While effective at curbing inflammation, dexamethasone appears to inhibit arginase-1 release in neutrophils, posing a double-edged sword for treatment strategies.
Broader Relevance
The implications of these findings extend far beyond COVID-19. Neutrophil behavior can significantly influence outcomes in various severe diseases, including cancer and autoimmune disorders. Dr. Amrita Dwivedi, a joint-first author of the study, articulated the broader relevance: "The insights gained from understanding neutrophil behavior in severe infections can spark further investigation into their roles across various health crises."
Conclusion
In conclusion, as the medical community continues to grapple with the evolving challenges posed by COVID-19, this research underscores the importance of examining often-overlooked elements of the immune response. From paving the way for innovative therapeutic strategies to understanding long-term patient care for those recovering from severe COVID-19, the study on neutrophils may unlock new dimensions in managing an ongoing global health crisis. As we strive to enhance clinical outcomes, the role of these previously understudied immune cells may prove to be pivotal in shaping the future of infectious disease treatment. Stay tuned as we delve deeper into this science!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)