Unveiling the Hidden Dangers: The Alarming Link Between Depression and Cardiovascular Disease in Cancer Patients
2025-03-31
Author: Li
Recent research reveals a shocking connection between depression and cardiovascular disease (CVD) among cancer patients—a finding that could reshape the way healthcare providers treat this vulnerable population. With CVD and cancer jointly occupying the top two spots among global mortality causes, public health systems are confronting a dual crisis that demands immediate attention. A staggering 32% of global deaths were attributable to CVD in 2019, while cancer accounted for 16.8%. Now, new evidence suggests that mental health noticeably intensifies these risks.
The Complexity of Cancer and Cardiovascular Health
The intersection of cancer and cardiovascular health represents a complex clinical challenge. Beyond the evident links, such as genetic mutations and chronic inflammation, cancer treatments are often a double-edged sword, potentially catapulting patients into heightened cardiovascular risk. For instance, chemotherapeutic agents like anthracyclines can lead directly to heart damage, while radiation therapy can cause severe arterial damage, creating a path for coronary artery disease.
The Weight of Depression in Cancer Patients
Adding to this turmoil is the psychological weight of a cancer diagnosis. A significant number of cancer patients, ranging from 15% to 25%, experience depression during their treatment journey. This mental health crisis not only hinders recovery but also accelerates cardiovascular deterioration through mechanisms like chronic inflammation and disruption of neurohormonal balance. Research indicates that depression can worsen cardiovascular health, leading to increased morbidity and mortality among cancer survivors.
Advancing Cardio-Oncology
In response to this healthcare quandary, the emerging field of cardio-oncology is gaining traction, focusing on the intersection of cardiovascular health and cancer treatment. Tools such as the Cardiometabolic Index (CMI) have been developed to gauge cardiovascular risk more effectively, particularly for patients undergoing androgen deprivation therapy or those treated with immune checkpoint inhibitors. Such approaches may provide a more holistic understanding of how psychological factors interplay with physical well-being.
Cardiovascular Mortality in Cancer Survivors
Surprisingly, recent studies suggest that the cardiovascular mortality rates among cancer survivors can overshadow cancer-specific mortality, particularly in breast and prostate cancer populations. In fact, a longitudinal analysis revealed that after ten years, those who survived certain cancers were more likely to succumb to cardiovascular-related issues than to their initial malignancies.
The Impact of Treating Depression
The stakes are high; a retrospective cohort study indicates that treatment for depression in lymphoma survivors led to a remarkable 38% reduction in heart failure risk. As a result, integrating routine depression screenings in cancer care is gaining advocacy, driven by evidence suggesting that addressing mental health can yield significant improvements in cardiovascular outcomes.
The Need for Integrated Care
Moreover, the unique cardiotoxic environment created by cancer therapies can amplify the risk factors associated with both conditions. This expanded understanding suggests that to truly support cancer patients, the healthcare system must prioritize mental health alongside physical health, paving the way for innovations in treatment protocols.
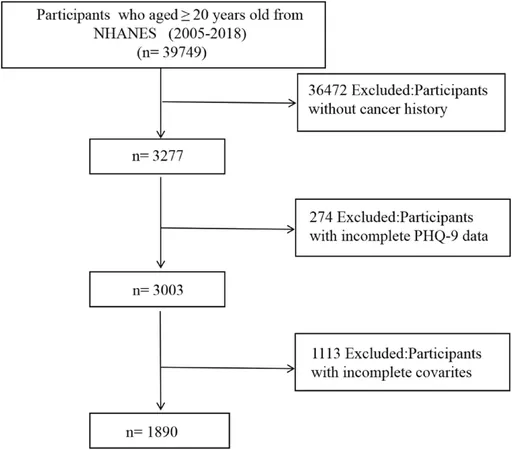
Data Insights from NHANES
Data from the National Health and Nutrition Examination Survey (NHANES) (2005-2018) provides vital insights, analyzing 1,890 cancer patients and demonstrating how the prevalence of CVD significantly correlates with rising levels of depressive symptoms. The analysis showed a clear connection: higher PHQ-9 scores—which assess depression—are associated with an elevated risk of cardiovascular incidents.
Conclusions and Future Research
Our findings reveal a critical link that could influence future healthcare protocols and clinical guidelines. This research highlights the urgent necessity for integrated care approaches that recognize and treat the complex interplay between mental and cardiovascular health in cancer patients.
As we continue to unravel the intricate relationship between depression and cardiovascular risk, it’s clear that proactive intervention strategies are essential. Understanding that managing mental health could lead to improved physical outcomes emphasizes the need for comprehensive patient care that addresses heart health as seriously as cancer treatment itself.
In conclusion, the evidence is mounting—cancer patients grapple with a dual health threat. Addressing depression is not merely about improving their mental state; it could be a pivotal factor in safeguarding their cardiovascular health and ultimately their survival. If we proceed with a holistic perspective, we can better protect these patients from the precipice of both depression and cardiovascular disease, steering them towards a healthier, more integrated future.
 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)