Unveiling the Hidden Link Between Diet and Gastrointestinal Cancers: What NHANES Data Reveals!
2024-10-09
Author: Rajesh
Unveiling the Hidden Link Between Diet and Gastrointestinal Cancers!
Gastrointestinal (GI) cancers, which encompass gastric cancer, liver cancer, esophageal cancer, pancreatic cancer, and colorectal cancer, have been a significant focus of public health due to their rising incidence and mortality rates globally. According to the World Health Organization (WHO), colorectal cancer alone accounts for over a quarter of cancer cases worldwide and is responsible for one-third of cancer-related deaths. Alarmingly, gastric cancer ranks as the second most common cause of cancer fatalities globally.
While smoking and alcohol consumption are well-known contributors to cancer risk, recent research underscores the pivotal role of dietary habits in the development of GI cancers. This growing body of evidence highlights the need for dietary modifications and emphasizes that dietary choices are vital modifiable factors in mitigating cancer risk.
Diet can affect cancer risk through various mechanisms, including altering the gut microbiome, influencing oxidative stress levels, and impacting energy balance. The Dietary Inflammatory Index (DII) and Dietary Oxidative Balance Score (DOBS) are two pivotal tools that assess the inflammatory and oxidative potential of diets. While a high DII, characterized by pro-inflammatory components, is linked with diets high in processed sugars and unhealthy fats, a low DII and a high DOBS are often associated with diets rich in fruits, vegetables, and whole grains—foods known to combat inflammation and oxidative stress.
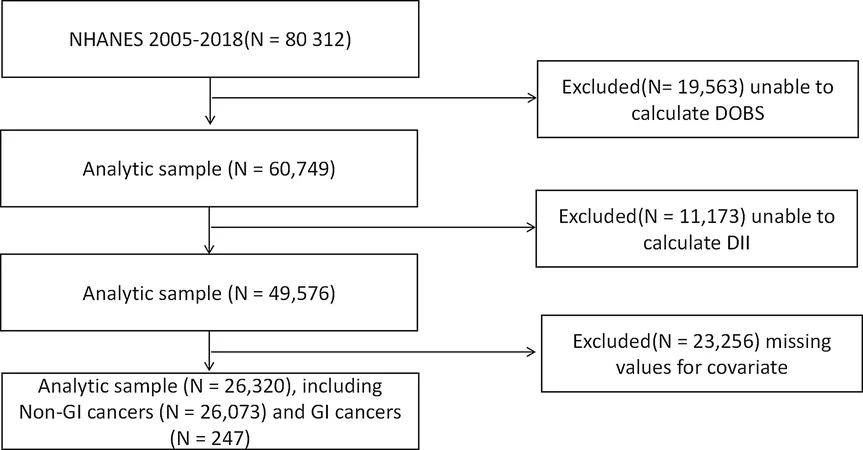
In a pioneering study using data from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018, researchers meticulously analyzed the correlation between DII, DOBS, and the incidence of GI cancers. They constructed logistic regression models and assessed the mediating roles of serum albumin and red cell distribution width (RDW)—both significant biomarkers of inflammation and nutrition.
The extensive study sample comprised 26,320 participants, analyzing the dietary patterns through detailed recall questionnaires and assessing serum biomarkers carefully stored for analysis. The results revealed comprehensive associations: a higher DII was significantly linked to an increased risk of GI cancers, whereas a higher DOBS showed a protective effect against these cancers.
Notably, the findings indicated that elevated serum albumin and RDW levels significantly mediated the connection between dietary factors and GI cancer risk. This intricate interplay suggests that maintaining a balanced diet with anti-inflammatory and antioxidant properties could be potentially life-saving.
Subgroup analyses revealed that the positive association between DII and GI cancers was particularly pronounced among younger and obese participants, while a high DOBS provided greater protective benefits for those without diabetes.
This research provides groundbreaking insights into the complex relationship between dietary factors and GI cancers. It serves to underscore the importance of a balanced dietary approach rich in anti-inflammatory and antioxidant foods, advocating for dietary interventions as vital preventative strategies against GI cancers.
In conclusion, this study not only illuminates the role of dietary patterns in influencing cancer risk but also encourages the implementation of dietary strategies as a cornerstone in the fight against GI cancers. As research progresses, it becomes increasingly evident that what we eat profoundly impacts our long-term health and susceptibility to chronic diseases. Therefore, individuals should consider evaluating and optimizing their diets to enhance their overall well-being and potentially prevent serious health risks, including cancer.
Stay tuned as we continue to uncover more about the significant impacts of nutrition on health outcomes!


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)