Unveiling the Struggles: Contraceptive Use and Chronic Conditions in Bangladesh
2025-04-05
Author: Wei
In an era where chronic health conditions such as diabetes and hypertension are on the rise, affecting over 1.5 billion individuals globally, the challenges faced by those living with these diseases are becoming increasingly apparent. Notably, about two-thirds of these individuals reside in low- and lower-middle-income countries (LMICs), like Bangladesh, where the prevalence of these conditions is climbing at an alarming rate. Factors such as genetics, aging, urbanization, lifestyle shifts, and obesity substantially contribute to this growing health crisis.
For women diagnosed with diabetes and hypertension, the stakes are particularly high during pregnancy, as they face increased risks of complications. This makes effective management of their health conditions and access to suitable contraceptive methods not just important, but crucial. Alarmingly, in Bangladesh, nearly half of diabetes and hypertension cases remain either undiagnosed or uncontrolled, leaving many unaware of their health status. Cultural perceptions often frame these conditions as afflictions of the affluent, further obscuring the reality that many affected individuals are younger and from economically disadvantaged backgrounds.
As educational levels rise, more Bangladeshi women are delaying pregnancies, often after pursuing higher education and establishing professional careers. However, as diabetes and hypertension emerge at younger ages, an increasing number of women find themselves at risk during pregnancy, often without prior knowledge of their conditions. The result is a concerning cycle of unplanned pregnancies, which can lead to dire health outcomes for both mothers and their children, including maternal and infant mortality.
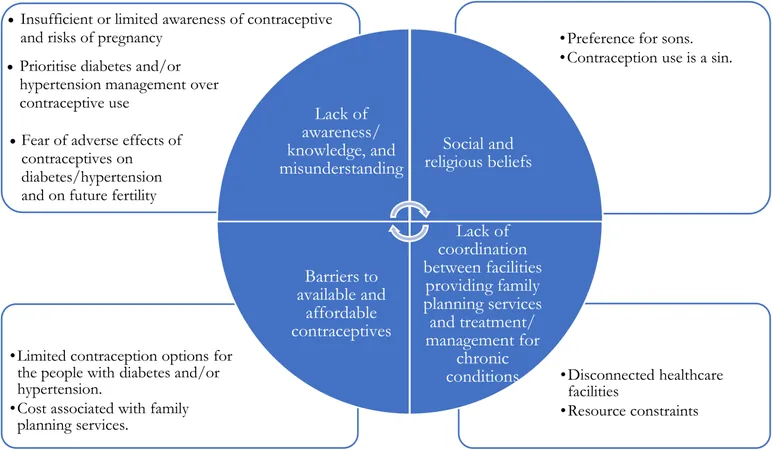
Despite the pressing need, the integration of contraceptive use into the management of chronic conditions in Bangladesh faces numerous obstacles. The healthcare system is characterized by fragmentation, with services delivered by government bodies, NGOs, and private providers—often in disjointed ways. This makes it difficult for those affected by chronic conditions to access comprehensive care. Limited awareness of effective contraception further complicates this landscape, especially among both patients and healthcare providers.
A qualitative study aimed at understanding the barriers to contraceptive use among people living with diabetes and hypertension in Bangladesh has illuminated several key issues. Participants reported significant misunderstandings regarding contraception’s role in managing their health conditions. Many believed that their chronic illnesses inherently decreased the likelihood of pregnancy, leading to a hesitance to use contraceptives.
Social and religious beliefs also emerged as significant barriers. Many respondents expressed a preference for male children—prompting them to avoid contraception in hopes of having sons. Moreover, misconceptions linking contraceptive use with religious sinfulness were prevalent. Notably, a staggering majority of participants were unaware that using contraception could be beneficial to their health, particularly regarding the management of diabetes and hypertension.
Other issues included the availability and affordability of contraceptives, with many reporting a lack of suitable options tailored for individuals with chronic health conditions. Financial burdens compounded these challenges, as families struggled to balance medications for their chronic illnesses with costs associated with contraceptives. The logistical nightmare of navigating multiple healthcare facilities for treatment and family planning solutions added to the frustration, resulting in many forgoing essential services altogether.
This study not only sheds light on the barriers faced by individuals with chronic conditions in Bangladesh but also echoes similar trends seen in other LMICs, calling for urgent policy interventions. Greater integration of contraceptive services within chronic disease management programs, along with community education initiatives, could significantly enhance access and awareness. Addressing these interconnected challenges is essential not only for improving maternal and child health outcomes but also for advancing towards global health goals.
By overcoming these barriers, Bangladesh has the opportunity to significantly improve the quality of life for those living with diabetes and hypertension, ensuring healthier futures for families across the nation.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)