Why "Pregnancy Loss" is Preferred Over "Miscarriage": Insights from Recent Research
2024-11-21
Author: Wei
Introduction
A groundbreaking study led by researchers at University College London (UCL) reveals that language surrounding pregnancy loss significantly impacts patients' mental health and emotional recovery. The findings suggest that terms like "pregnancy loss" are generally more accepted than "miscarriage" among individuals who have experienced this traumatic event.
Research Overview
This comprehensive research, the first of its kind, involved interviews with 391 participants from across the UK, all of whom had lived experience of pregnancy loss. The study, spearheaded by Dr. Beth Malory from UCL's English Language & Literature department, offers critical insights into how language can influence emotional well-being during a profoundly difficult time.
Previous Work
Building on previous work published in September, where responses from 339 individuals—including patients and healthcare professionals—were analyzed, this latest study emphasizes the importance of personalized communication in healthcare settings. In collaboration with national pregnancy and baby loss organizations such as Tommy's and Sands, the research team aimed to underscore how language can affect patients' experiences of loss and the need for sensitivity in communication.
Statistics on Pregnancy Loss
Statistics reveal that more than one in six pregnancies in the UK end in loss each year, raising awareness among clinicians and charities about the detrimental effects of certain terminologies. Participants in the study expressed feelings of confusion and fear when confronted with clinical terminology that lacked sensitivity, highlighting the urgent need for healthcare providers to accommodate individual language preferences.
Distressing Terminology
Terms like "abortion," "feticide," and "termination" were noted as particularly distressing when describing medical procedures following a pregnancy loss. Additionally, phrases such as "incompetent cervix" were linked to feelings of guilt and self-blame. Moreover, words such as "blighted ovum," "empty sac," and "chemical pregnancy" evoked strong negative emotions, leading participants to feel inadequate or that their loss was minimized.
Participant Testimonials
One participant poignantly noted, "The language used during my first pregnancy loss was horrific and inappropriate. This led to increased trauma around my loss." Such testimonials reinforce the need for healthcare practitioners to exercise caution in their wording and offer alternatives that respect the patients’ emotional states.
Key Recommendations
The research culminated in four key recommendations for clinicians dealing with pregnancy loss: 1. Recognize the power of language. 2. Inquire about language preferences when uncertain. 3. Employ softer terminology in clinical discussions. 4. Prioritize respect for patient preferences.
Analysis of Clinical Language
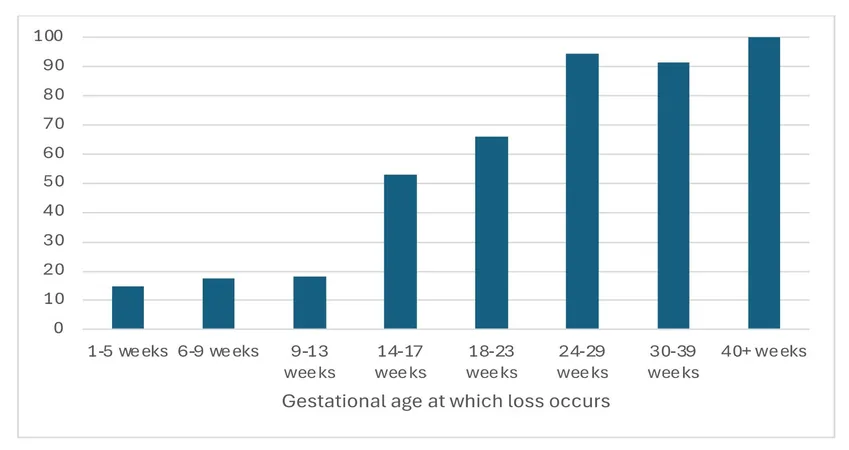
The study also analyzed the specific language currently used in clinical settings, with notable findings: 62% of respondents found the term "miscarriage" acceptable if the loss happened before 24 weeks, while a striking 81.6% considered "pregnancy loss" an acceptable term at any stage of pregnancy. Conversely, terms such as "cervical incompetence" garnered unacceptability ratings of over 80%.
Conclusion
Dr. Malory emphasized that these findings pave the way for evidence-based recommendations on language choice, aiming to mitigate harm to those facing the emotional turmoil of pregnancy loss. The message to policymakers and writers is clear: choosing compassionate and considerate language can make a significant difference in the lives of those affected.
As society navigates sensitive topics like pregnancy loss, understanding and utilizing language that respects individuals’ experiences becomes crucial. We must balance clinical precision with emotional sensitivity—a challenge that will undoubtedly require ongoing dialogue and reflection within the medical community and beyond.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)