Bridging the HIV Treatment Gap: Progress Made and Challenges Ahead
2024-12-09
Author: Benjamin
The Journey of HIV Treatment: A Historical Perspective
The beginning of what would come to be recognized as a global health crisis can be traced back to June 5, 1981, when a report outlined cases of five homosexual men suffering from a rare form of pneumonia, Pneumocystis carinii pneumonia. The investigation revealed these cases were linked to the Human Immunodeficiency Virus (HIV). Since that time, remarkable advancements in prevention and treatment have improved the lives of countless individuals living with HIV, thanks largely to the development of antiretroviral therapies (ART).
The FDA approved its first treatment, Zidovudine (AZT), in 1987, marking a significant milestone in the fight against HIV. A major breakthrough occurred in 1995 with the introduction of Highly Active Antiretroviral Therapy (HAART), often referred to as combination antiretroviral therapy (cART), which significantly altered the prognosis for HIV-positive individuals.
Current Landscape: Progress and Disparities
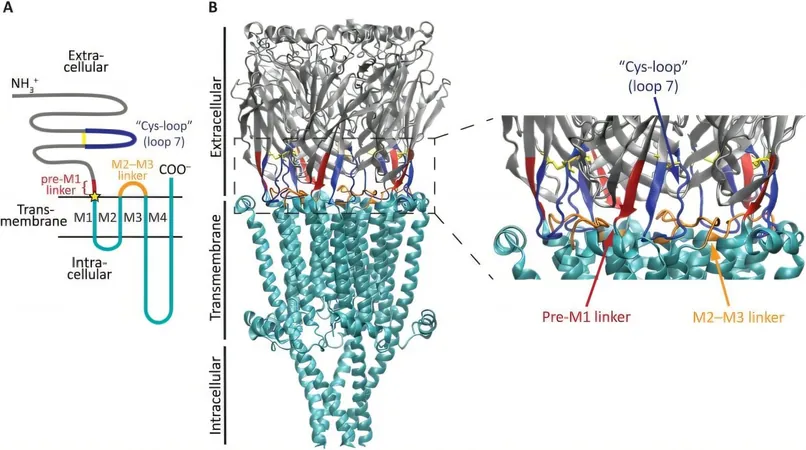
Despite these advancements, challenges remain, particularly access to effective HIV treatment services. Approximately 65% of the 39.9 million people living with HIV reside in sub-Saharan Africa, where healthcare inequities persist. The introduction of generic antiretroviral therapies in 2001 has improved accessibility, yet these treatments merely suppress the virus rather than providing a cure—largely due to the presence of latent reservoirs in memory CD4 T cells.
Hope lies in notable cases like the “Berlin patient,” who, after undergoing two stem cell transplants from a donor with a CCR5-Δ32 mutation—an alteration that effectively shields CD4 T cells from HIV—has cleared the virus. Furthermore, there are individuals known as long-term non-progressors (LTNPs) and elite controllers (ECs) who manage the virus without the need for treatment.
Researchers are currently exploring innovative avenues such as stem cell transplantation, genetically engineered CD4 T cells resistant to HIV, and strategies to bolster the immune system. However, practical solutions must minimize toxicity and be geared toward achieving a global reach. Alarmingly, less than one-third of people living with HIV are currently achieving viral suppression, highlighting the urgent need for more effective interventions. A potential cure would mainly benefit those with an undetectable viral load—an estimated 25% in high-income countries and significantly lower in low-income regions.
Closing the Healthcare Divide: Effective Strategies
To effectively bridge the existing gaps in healthcare, we must concentrate on several strategic areas:
1. **Community Engagement:** Non-governmental organizations (NGOs) must work closely with local communities to implement targeted screening programs for vulnerable populations, including men who have sex with men, injectable drug users, and sex workers.
2. **Enhanced Access to Prevention:** It is essential to improve access to successful preventive measures, including: - Strategies to prevent mother-to-child HIV transmission. - The provision of pre-exposure prophylaxis (PrEP) to reduce infection risk. - Access to post-exposure prophylaxis (PEP) for those who may have been recently exposed to HIV.
3. **Investment in ART and Research:** Continued financial commitment to antiretroviral treatment is crucial, as is the drive for effective vaccine development and advanced therapeutic options.
These efforts, when effectively implemented, can significantly close the healthcare gap and lead to better health outcomes for marginalized populations.
Looking Ahead: A Vision for the Future
The World Health Organization (WHO) has set ambitious goals to ensure that by 2025, 95% of individuals living with HIV are diagnosed, 95% of those diagnosed receive ART, and 95% of treated individuals achieve viral load suppression. Achieving these targets can not only improve individual health outcomes but also greatly reduce rates of HIV transmission globally.
With a resolute commitment to innovative approaches and enhanced community-based strategies, we are on the brink of closing the gaps in HIV treatment. A united effort is crucial for forging a healthier future for all. Will we rise to the challenge?








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)