Shocking Rise of Drug-Resistant Bacteria in Hospitals Puts Newborns at Risk Across Six Countries
2024-11-21
Author: William
A groundbreaking study reveals a frightening rise in drug-resistant bacteria lurking on hospital surfaces in six low- and middle-income countries. This alarming investigation could impact newborns at unprecedented rates, especially in regions where healthcare resources are scarce.
Antimicrobial resistance (AMR) occurs when bacteria develop the power to withstand treatments from antibiotics or other antimicrobial medications, leading to infections that are increasingly hard to treat. Common infections like pneumonia, urinary tract infections, and sepsis—all typically treated with antibiotics—are becoming more dangerous.
Newborns, with their still-developing immune systems, are particularly vulnerable. The research highlights a grim statistic: infections among newborns are 3 to 20 times higher in low- and middle-income countries compared to their wealthier counterparts. In 2020, an estimated 2.4 million newborns succumbed to sepsis within their first month of life, with the majority of these deaths occurring in sub-Saharan Africa.
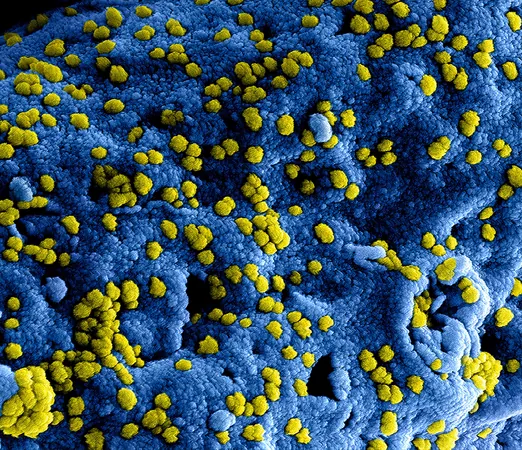
The study, spearheaded by the Ineos Oxford Institute for Antimicrobial Research, focused on 10 hospitals in Bangladesh, Ethiopia, Nigeria, Pakistan, Rwanda, and South Africa. Researchers collected approximately 6,290 surface swabs from critical care areas such as intensive care units for newborns and maternity wards. They notably detected high levels of bacterial contamination around sink drains—one of the dirtiest hotspots in hospitals.
The researchers discovered that surfaces were teeming with bacteria carrying antibiotic resistance genes, particularly genes that provide resistance to carbapenems, the last line of defense against severe infections in newborns.
Using whole genome sequencing, the team identified 18 different bacterial species on these hospital surfaces, including those notorious for causing pneumonia, urinary tract infections, and blood infections. Alarmingly, one bacterial strain found on surfaces matched a strain that caused sepsis in newborns at one of the hospitals. This correlation raises concerns about the potential transmission of resistant bacteria from hospital environments to vulnerable infants.
The capacity for bacteria to share resistance genes through horizontal gene transfer—where mobile DNA elements leap from one bacterium to another—complicates the situation. This process accelerates the spread of antibiotic resistance among bacteria present in close proximity on hospital surfaces, making treatments less effective and exposing patients to greater risks.
Experts stress the need for an urgent overhaul of infection prevention and control measures, emphasizing that effective strategies are particularly vital in low-resource settings. Practical steps such as ensuring access to safe drinking water, implementing comprehensive vaccination programs, and establishing rigorous protocols for cleaning and maintaining hospital surfaces can significantly reduce infection risks.
However, many hospitals in these countries struggle with underfunding. Without the necessary financial backing from governments and global health organizations, implementing these critical measures remains a daunting challenge.
Failure to address these issues threatens to lead to an unprecedented public health crisis, with infections not just rising, but becoming untreatable. Accessible and sustainable infection control measures could save thousands of lives, particularly among the most vulnerable—newborn infants.
This research not only highlights the global challenge of antimicrobial resistance but also calls for immediate attention to safeguard the health of future generations. The stakes could not be higher, and action must be taken now to prevent a potential healthcare disaster.






 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)