Surprising Findings: Anticholinergics May Lower Mortality in Parkinson’s Disease Without Raising Hip Fracture Risk!
2024-11-18
Author: Michael
Introduction
The relationship between antiparkinsonism anticholinergics (AAs) and the risk of hip fractures in patients with Parkinson’s disease (PD) has long been a subject of debate. A recent retrospective cohort study based on Taiwan's National Health Insurance Database provides crucial insights, suggesting that these medications could not only be safer than previously thought but also associated with lower mortality.
Study Overview
The study analyzed a sizeable cohort of newly diagnosed PD patients aged 50 and above between 2000 and 2015, categorizing them based on their exposure to anticholinergic drugs. The results revealed alarming trends in hip fracture rates across groups but also threw light on a possibly lesser-known benefit of AAs.
Methods and Findings
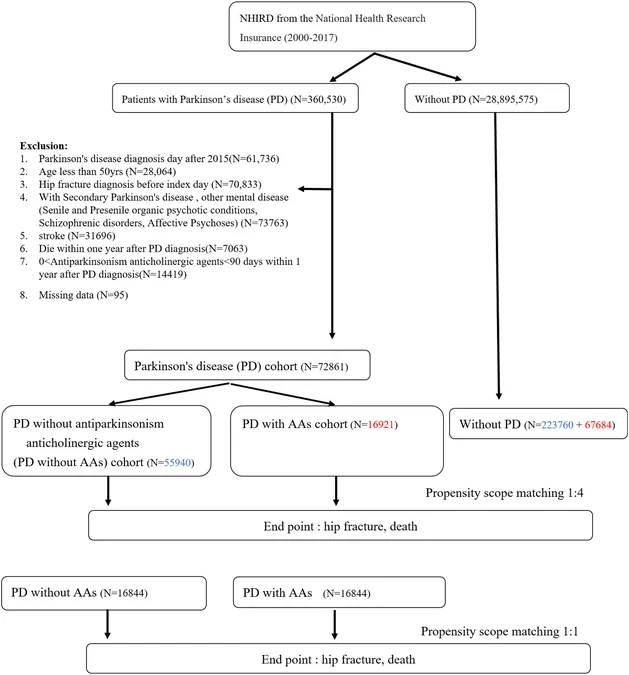
Researchers segmented 72,861 participants into three groups: those with PD who used AAs for over 90 days (16,921), those without AAs (55,940), and matched non-PD controls (291,444). The study utilized advanced statistical models to consider competing risks - both hip fractures and mortality - revealing a striking finding: 1. **Hip Fracture Risk:** Both groups with PD showed elevated risks of hip fractures when compared to non-PD controls, with adjusted hazard ratios of 1.51 (PD with AAs) and 1.53 (PD without AAs). However, a significant conclusion emerged: there was no additional risk of hip fractures associated with AAs when comparing PD patients on AAs to those not using them. 2. **Mortality Rates:** Mortality was notably higher in both PD cohorts compared to their non-PD counterparts, with adjusted hazard ratios of 2.24 for those on AAs and 2.44 for those without. Intriguingly, PD patients using AAs had a lower mortality rate compared to those who did not use them, with an adjusted hazard ratio of 0.93.
Conclusion and Implications
This large-scale study demonstrates that while patients with PD possess a heightened risk for hip fractures and mortality, the use of AAs does not exacerbate fracture risk and may even correlate with improved survival outcomes. These findings challenge the prevailing narrative suggesting that anticholinergics pose greater risks for hip fractures, thereby calling for further research into their potential benefits. As healthcare professionals continue to navigate treatment strategies for Parkinson’s disease, this study underscores the importance of individualized patient care and highlights the necessity for careful examination of medication risks versus benefits.
Call to Action
As the conversations around Parkinson's disease treatment evolve, patients and caregivers should stay informed about the latest findings. This research serves as a critical reminder that assumptions about medication safety may not always align with the evidence. Future prospective studies are desperately needed to explore these associations in greater depth, potentially transforming clinical guidelines for managing Parkinson’s disease. Stay tuned as we continue to monitor this developing story and dive deeper into the emerging research surrounding Parkinson’s disease and its treatments!



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)