The Alarming Link Between COVID-19 and New-Onset Dementia: What You Need to Know!
2024-12-15
Author: Jacques
Introduction
The COVID-19 pandemic, triggered by the novel coronavirus SARS-CoV-2, has drastically altered global health landscapes, impacting not just immediate health concerns but also long-term neurological outcomes. Researchers have increasingly focused on how COVID-19 could increase the risk of cognitive decline and even lead to the onset of neurodegenerative dementia among older adults.
Correlation Between COVID-19 and Cognitive Issues
Recent studies have suggested a disturbing correlation between COVID-19 infection and a heightened risk of cognitive issues, significantly affecting older populations. Compared to those recovering from other respiratory diseases or healthy older adults, those infected with COVID-19 show an alarming propensity for "brain fog," dementia, and worsening pre-existing cognitive conditions, such as Alzheimer's disease. These findings challenge our understanding of how acute infections might shape the future neurological health of our most vulnerable populations, particularly during the ongoing pandemic.
Underlying Biology
The underlying biology may offer clues. Evidence has emerged indicating that SARS-CoV-2 can instigate inflammation in the brain, disrupt neurological functions, and even accelerate the progression of dementia. In particular, COVID-19 has been linked to severe inflammatory responses, aggregation of tau proteins (a hallmark of Alzheimer's), and increased levels of neurofilament light chain—proteins associated with neuronal injury. Furthermore, the impact of COVID-19 on the brain's blood vessels—including ischemia and thrombus formation—might mirror the mechanisms of vascular dementia.
Impact on Older Adults
Studies indicate that older adults who have pre-existing cardiovascular conditions are disproportionately affected, experiencing significantly compounded risks for cognitive deterioration post-COVID-19. Nonetheless, research in this area remains disjointed, utilizing varying methodologies and yielding mixed results, particularly about different age groups within older populations.
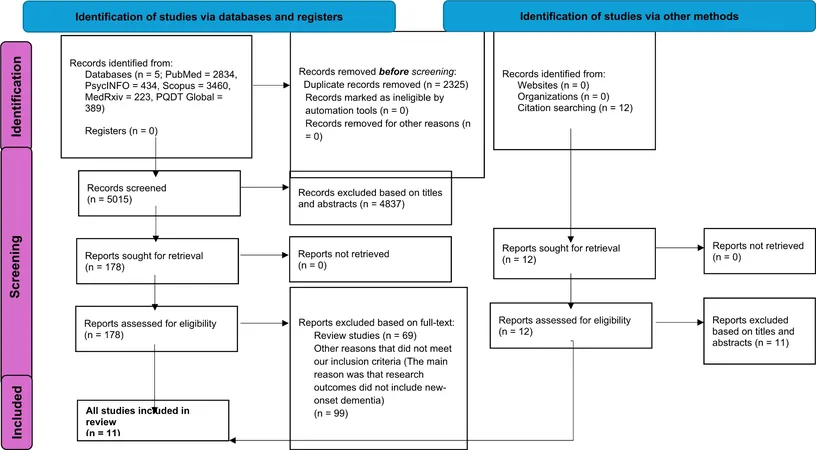
Systematic Review and Meta-Analysis
A systematic review and meta-analysis aimed to fill this knowledge gap by rigorously evaluating existing studies examining the impact of COVID-19 on new-onset dementia in older adults (aged 60 and above). Conducting comprehensive searches across major medical databases, researchers analyzed data from over 939,824 COVID-19 survivors compared to more than 6 million controls from 11 studies.
Findings of the Study
The review found that approximately 1.82% of older adults post-COVID developed new-onset dementia, a striking increase compared to just 0.35% in non-COVID controls, suggesting an almost five-fold increased risk. This finding is significant as it highlights the potential long-term cognitive toll of COVID-19, which could have profound implications for families, healthcare systems, and economies worldwide.
Subgroup Analyses and Gender Differences
The results of subgroup analyses revealed that the risk of developing new-onset dementia was particularly pronounced at 12 months following COVID-19 infection. Outpatients were found to have a 91% increased risk, while hospitalized patients faced a staggering threefold risk of developing dementia compared to those without COVID-19. Furthermore, the gender differences within the studies indicated that women in both COVID-positive and control groups exhibited higher dementia risks, suggesting that while COVID-19 infection may exacerbate conditions in both sexes, it does not seem to disproportionately target one gender over another.
Conclusion and Urgent Need for Intervention
Importantly, this research emphasizes the urgent need for early intervention strategies. With projections indicating that the global burden of dementia could triple by 2050, understanding the ramifications of COVID-19 on cognitive health is becoming increasingly crucial. As we navigate the tail end of a global pandemic, this analysis serves as a stark reminder of the potential long-term implications of COVID-19 on our aging population, highlighting the necessity for continued vigilance, further research, and perhaps most critically, an emphasis on vaccine uptake and preventative measures.
Final Thoughts
In summary, the data suggests that avoiding COVID-19 could be a protective factor against the risk of dementia. The findings of this review not only serve to deepen our understanding of the links between viral infections and cognitive health but also compel us to consider the long-lasting effects of pandemics on vulnerable populations. Each infection could herald new challenges as the world grapples with the health legacy of COVID-19. Stay informed, stay safe, and let's hope that future research continues to shed light on these critical issues.







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)