Unveiling the Hidden Challenges of Empty-Nest Older Adults in China: New Insights into Intrinsic Capacity
2024-12-19
Author: Amelia
Introduction
In an aging world, the plight of older adults, particularly those living alone, is increasingly concerning. With China now hosting one of the largest populations of elderly individuals—over 145 million empty-nest older adults as of 2020—urgent action is required to address the unique challenges they face. The latest studies have indicated that these individuals are prone to cognitive decline, higher rates of disability, and significant mental health issues compared to their non-empty-nest counterparts. One alarming trend is the rising incidence of older adults dying alone, amplifying the need for effective support strategies.
Intrinsic Capacity: A Beacon of Hope
Intrinsic capacity (IC)—the cumulative mental and physical capabilities of older adults—plays a crucial role in their overall health and quality of life. Defined across various domains including sensory, cognitive, locomotion, psychological well-being, and vitality, IC acts as a cornerstone for successful aging. Research has demonstrated that a robust IC can mitigate risks related to falls, hospitalizations, and even mortality. Alarmingly, declines in IC can correlate with reduced quality of life, increased frailty, and escalated healthcare needs.
Despite existing focus on individual factors influencing IC, a gap remains—particularly concerning the factors impacting empty-nest older adults. Through the lens of the health ecology model, which encompasses personal traits, psychological behavior, interpersonal networks, living conditions, and the policy environment, this study delves deeper into understanding these individuals' needs.
Latent Class Analysis: Unmasking Subgroups
The research uniquely employed latent class analysis (LCA) to identify differentiated subgroups among the older population based on their IC. This novel approach allows for tailored healthcare interventions, addressing the specific requirements of various cohorts within the empty-nest demographic.
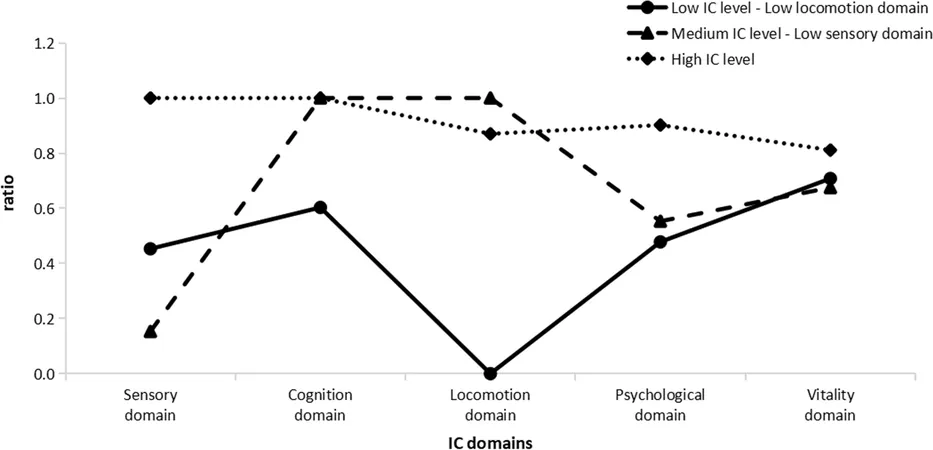
Findings revealed three primary subclasses among participants:
1. Low IC Level—Low Locomotion Domain: Comprising 33.5% of older adults, this group showed significant declines across all IC domains, particularly in locomotion.
2. Medium IC Level—Low Sensory Domain: Making up 16.9%, individuals here exhibited moderate overall IC with notable impairments in sensory functions.
3. High IC Level: The largest group at 49.6%, these older adults enjoyed good health across all IC domains.
These subgroups underline the pressing necessity for customized interventions targeting locomotion-related issues, especially for those with low IC levels.
Key Influencing Factors on Intrinsic Capacity
The study uncovered several critical factors impacting IC, including age, marital status, frequency of child visits, and the presence of multimorbidity. Notably:
- Older adults with multiple chronic illnesses tend to have lower IC. This correlation stresses the need for comprehensive healthcare strategies focusing on disease management.
- Individuals with a spouse or frequent visits from children exhibited better IC levels, reinforcing the importance of familial connections in supporting aging adults.
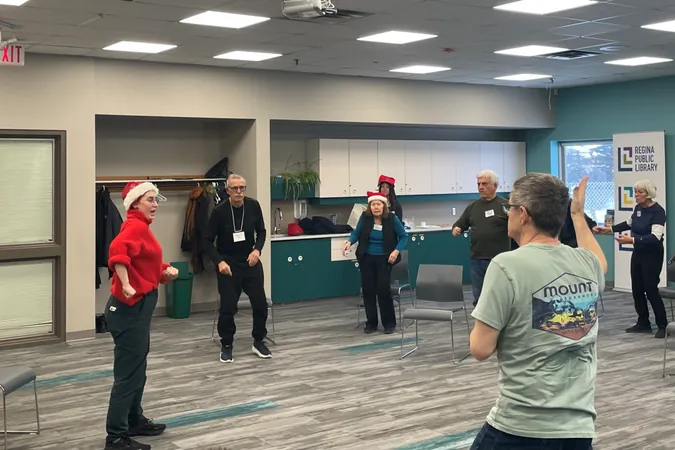
Furthermore, social networks significantly affect the well-being of empty-nest seniors. As social isolation can exacerbate feelings of loneliness and depression, fostering community ties is essential for promoting a higher quality of life.
Urgent Need for Personalized Interventions
This insightful study serves as a wake-up call for communities and healthcare providers. By applying the health ecology model alongside LCA methodology, we can move towards more nuanced, personalization-driven approaches that directly address the challenges faced by empty-nest older adults.
The findings underline the crucial need for targeted intervention strategies that not only improve IC but also enhance the overall life experience of this vulnerable population. Ensuring that older adults have robust support systems—including social engagement and healthcare management—could significantly delay functional decline, improve mental health, and elevate their quality of life.
Conclusion: A Call to Action!
The urgent call for action is clear: As the population of empty-nest older adults continues to grow, so too must our commitment to understanding their unique challenges and vulnerabilities. It is no longer sufficient to rely on broad healthcare strategies; instead, we must embrace personalized, evidence-based interventions to enhance their intrinsic capacity and ensure that they age with dignity and support.
As communities and healthcare professionals, let’s prioritize the development of tailored programs that address the multifaceted needs of this aging population. Together, we can create a future where every older adult thrives!







 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)