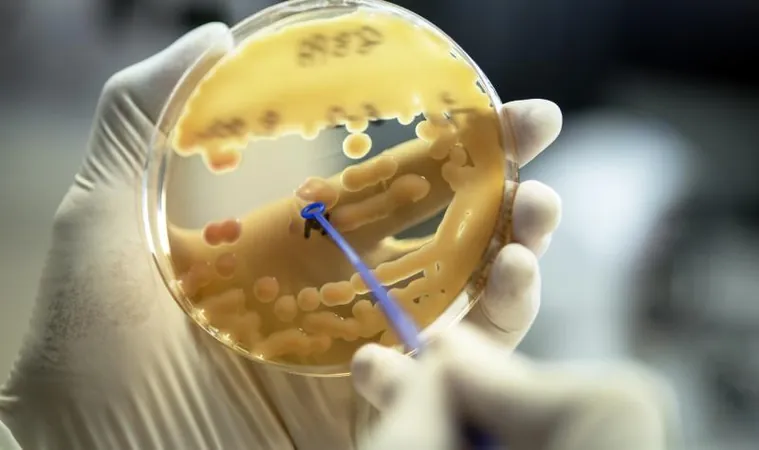
Alarming Surge in Antibiotic Resistance and Consumption in Europe: A Wake-Up Call
2024-11-18
Author: Li
Introduction
Recent data released by the European Centre for Disease Prevention and Control (ECDC) reveals a concerning trend: the European Union (EU) is failing to meet its targets for reducing antimicrobial resistance (AMR) and antibiotic consumption. This urgent situation was highlighted on European Antibiotic Awareness Day, emphasizing the gravity of the issue in 2023.
The Alarming Statistics
The statistics compiled by the European Antimicrobial Resistance Surveillance Network (EARS-Net) paint a bleak picture. There has been a staggering nearly 60% increase in bloodstream infections caused by carbapenem-resistant Klebsiella pneumoniae since 2019, raising alarms among health officials. The implications of this rise underscore not only the prevalence of these infections but also their potential resistance to current treatments.
Insights from ECDC
A press conference led by ECDC Director Dr. Pamela Rendi-Wagner revealed alarming statistics: over 35,000 individuals in the EU succumb to drug-resistant infections each year, and around 4.3 million patients acquire healthcare-associated infections during their hospital stays, many of which are antibiotic-resistant. Rendi-Wagner stressed the significant impact of AMR on patients and families, saying, "These numbers show one thing: that the problem is indeed huge."
Mixed Results in the EARS-Net Report
The EARS-Net report offers a mix of insights. On a slightly positive note, the incidence of methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections has decreased by 17.6% since 2019, reflecting some improvement measures. However, the incidence of serious infections caused by carbapenem-resistant Klebsiella pneumoniae has skyrocketed by 57.5%, far exceeding the 2030 target set by the EU Council. This trend puts increasing pressure on healthcare systems across the continent.
Geographical Disparities in AMR Rates
Dominique Monnet, head of ECDC's Antimicrobial Resistance and Healthcare-Associated Infections program, stated, "This poses a growing threat to patients in hospitals across the EU, in almost all member states." Alongside the alarming rise in Klebsiella infections, there has also been a reported increase in bloodstream infections caused by other resistant pathogens, including vancomycin-resistant Enterococcus faecium.
Call for Action
Geographically, AMR rates show significant disparities across the EU, with southern and southeastern countries reporting the highest incidence of drug-resistant infections. Dr. Rendi-Wagner remarked, "Europe is, overall, trending in the wrong direction." She emphasized the critical need for collaborative efforts among member states to harmonize progress and share effective solutions.
Recommendations for Hospitals
The ECDC is calling for hospitals to heighten their focus on infection prevention and control measures, which include improving hand hygiene, better screening for resistant bacteria, increased isolation capacity, and enhancing infection control personnel.
Increasing Antibiotic Consumption
Compounding the problem is the uptick in antibiotic consumption. The European Surveillance of Antimicrobial Consumption Network (ESAC-Net) reported a 1% increase in antibiotic usage compared to 2019, despite initial sharp declines observed during the COVID-19 pandemic. The average antibiotic consumption in 2023 reached 20.1 defined daily doses (DDD) per 1,000 inhabitants per day, which is significantly above the 2030 target aiming for a 20% reduction.
Sector-Specific Findings
The community sector accounted for the majority of antibiotic use, with penicillins represented as the most consumed group. While some countries made strides toward their 2030 targets, a concerning trend emerged: 14 nations registered increases in antibiotic consumption, with some experiencing rises in double digits.
The Way Forward
In light of these growing challenges, Dr. Rendi-Wagner called for renewed investment in the development of new antibiotics and urged enhanced antimicrobial stewardship efforts across both healthcare settings and the community. She stated, "Public health awareness campaigns targeting AMR are needed more than ever, complemented by social and behavioral interventions."
Conclusion
As Europe faces these escalating health threats, the call for collective action is louder than ever. It is imperative for public health officials, healthcare systems, and communities to unite in combating antibiotic resistance—a growing menace that endangers lives and challenges the very foundation of modern medicine.


 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)