Cervical Cancer Deaths in Young Women Plummet: A Major Public Health Triumph!
2024-11-27
Author: John Tan
Cervical Cancer Deaths in Young Women Plummet: A Major Public Health Triumph!
Recent research indicates a dramatic decline in cervical cancer deaths among young women in the United States, suggesting a major public health success story.
According to statistics from the National Center for Health Statistics, the number of women under 25 who died from cervical cancer dropped to just 13 between 2019 and 2021, compared to 35 deaths recorded between 2013 and 2015. This represents an astonishing 62% decrease in cervical cancer-related fatalities for this age group.
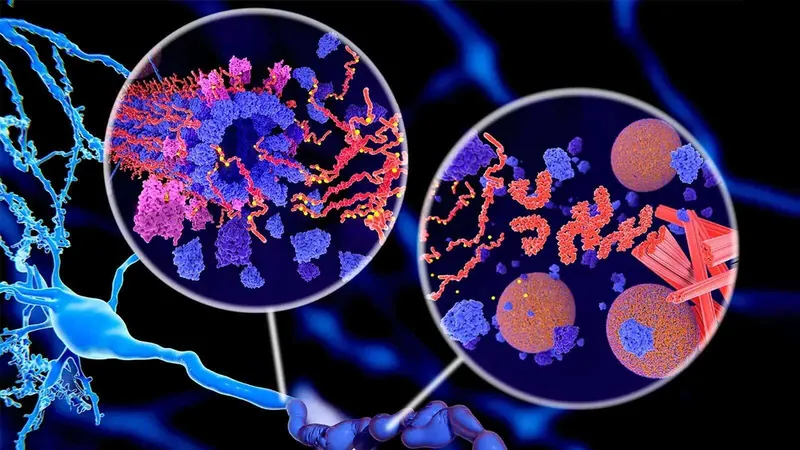
The study, published in the prestigious journal JAMA, marks a significant first, proposing that the HPV vaccine, introduced in the U.S. in 2006, is having a profound impact on cervical cancer mortality rates among young women. The vaccine works by preventing infections from high-risk strains of human papillomavirus (HPV), which is the leading cause of cervical cancer.
“This is a watershed moment in the public health success narrative for cervical cancer prevention,” said Ashish Deshmukh, the study's co-author and an associate professor at the Medical University of South Carolina. He emphasized the ongoing need to improve HPV vaccination rates across the nation.
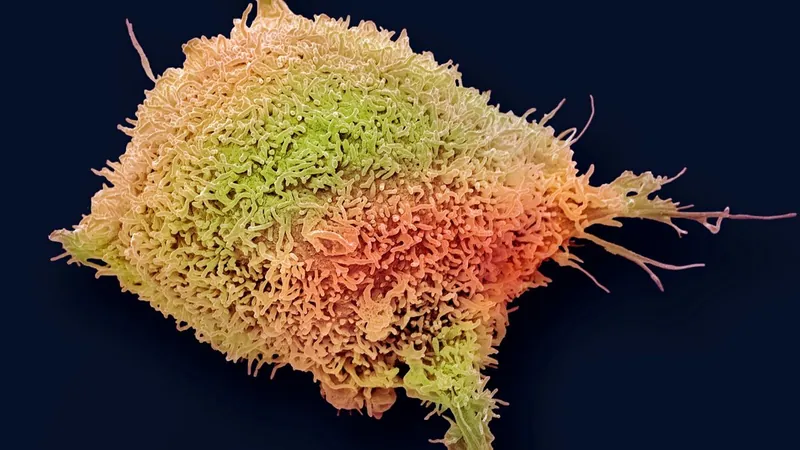
Cervical cancer affects the cervix—the lower part of the uterus connecting to the vagina—primarily linked to specific HPV strains altering cervical cell DNA, leading to uncontrolled growth. Although cervical cancer ranks as the fourth most common cancer in women worldwide, it is largely preventable with timely vaccination and regular screenings. Moreover, early detection offers the possibility of effective treatments such as surgery and chemotherapy, though striking disparities in healthcare mean that approximately 94% of cervical cancer deaths occur in low- and middle-income countries.
The Centers for Disease Control and Prevention (CDC) recommends that all children receive the HPV vaccine around ages 11 or 12, though vaccination can begin as early as 9 years old for certain at-risk groups. If unvaccinated in childhood, individuals can still receive the vaccine up to age 26 or beyond upon a doctor's advice. Typically, those vaccinated before age 15 require just two doses, while later vaccinations necessitate three.
Since the introduction of the HPV vaccine, vaccination rates in the U.S. have been steadily increasing, with 2023 data indicating that about 76.8% of adolescents aged 13 to 17 have received at least one dose. However, public health experts caution that these rates have stalled, remaining below the ambitious target of 80% set by the Office of Disease Prevention and Health Promotion—a goal originally aimed at being reached by 2020.
Though this latest study did not directly correlate vaccination rates with reduced cervical cancer deaths, previous research supports this association, linking increased vaccination coverage to decreased HPV infections and consequently fewer cervical cancer cases.
Dr. Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization, recently stated, “The elimination of cervical cancer is within our grasp.” He emphasized that unlike many other cancers, most cervical cancer cases and deaths are preventable. Tackling global disparities in access to HPV vaccines and diagnostic services could potentially enable the world to eliminate cervical cancer entirely.
As we celebrate this extraordinary progress, it's crucial to continue advocating for wider vaccine access and education to protect future generations from this disease. Will we finally eradicate cervical cancer? Only time—and our commitment to health equity—will tell.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)