Shocking Study Reveals Men's Brains Shrink 10 Years Earlier Due to Heart Risks!
2024-11-26
Author: Ming
Introduction
A groundbreaking study from the U.K. Biobank has unveiled a startling reality: men at high risk of cardiovascular disease experience brain volume changes an entire decade earlier than women. This discovery, led by Dr. Paul Edison from Imperial College London, reveals the urgent need for awareness around the impact of heart health on cognitive function, particularly in aging men aged 55 to 64.
Key Findings
The research particularly highlights the correlation between cardiovascular risks—such as obesity—and significant reductions in gray matter volume in men, compared to women, who begin to exhibit similar effects ten years later, at ages 65 to 74. This discrepancy raises critical questions about gender differences in health and aging.
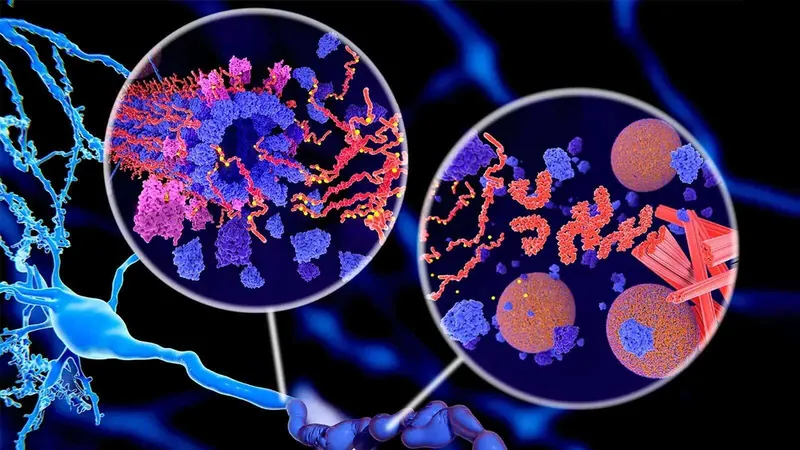
MRI scans have shown that men are far more susceptible to the cognitive decline associated with cardiovascular issues. “Men were more likely to be affected by the influence of cardiovascular risk on memory problems a decade earlier than women,” said Dr. Edison. The scans revealed alarming reductions in brain volumes, especially in regions essential for learning and memory located in the temporal lobes.
Impact of Modifiable Risk Factors
The researchers underscore that modifiable risk factors such as obesity are closely linked to an increased likelihood of developing dementia. However, this research sheds new light on how early cardiovascular risks uniquely affect men sooner than women. Dr. Edison suggests that differences in hormonal profiles, fat distribution, and lifestyle choices—including diet, smoking, and alcohol consumption—could contribute to this phenomenon.
Role of Estrogen
Estrogen, which has protective cardiovascular effects in women, may play a crucial role in delaying these cognitive declines. After menopause, many women see a notable rise in heart problems, which could explain why they experience similar brain changes a decade later than men. “The protective effect of estrogen pre-menopause may explain the delay in cognitive decline seen in women,” he highlighted.
Study Overview
The comprehensive study involved 34,425 participants averaging 64 years old, assessed through rigorous cardiovascular risk scoring. This included evaluations of cholesterol levels, blood pressure, and diabetes status, alongside brain and abdominal MRIs. The research employed advanced imaging techniques to meticulously analyze changes in brain volume associated with cardiovascular health.
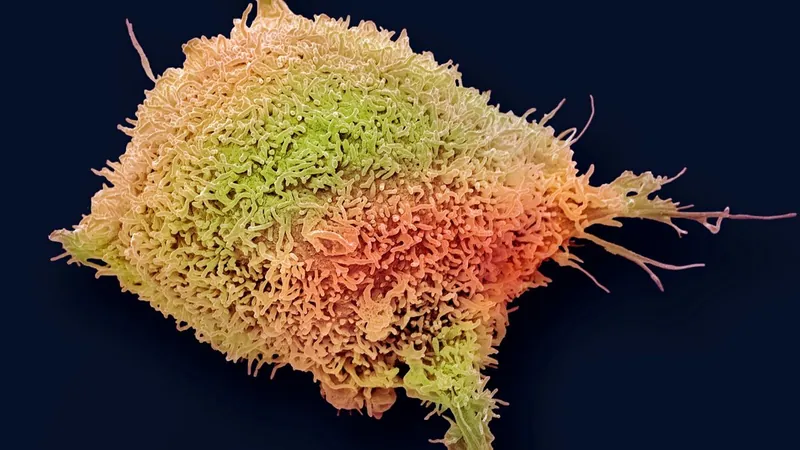
Neurodegeneration and Cardiovascular Risks
As participants aged, researchers observed a concerning bell-shaped relationship between cardiovascular risk and neurodegeneration. The negative impact of cardiovascular risk was pervasive throughout various cortical regions, stressing how heart health is intricately linked to cognitive abilities.
Call for Proactive Intervention
The study calls for a proactive approach to combating cardiovascular risks pre-emptively, emphasizing the importance of intervention before the age of 55. Aggressively targeting these health issues could significantly reduce the risks of neurodegeneration and ultimately combat Alzheimer's disease.
Emerging Treatments
Moreover, there's emerging hope in the potential repurposing of existing obesity and diabetes therapies as treatments for Alzheimer’s. Ongoing phase III clinical trials are testing promising drugs like semaglutide (marketed as Ozempic and Wegovy) against early Alzheimer’s disease, alongside other medications such as anti-hypertensives and metformin.
Conclusion
While the U.K. Biobank data lacks specific Alzheimer's biomarkers, the findings emphasize the necessity of understanding how cardiovascular risk factors uniquely influence various neurodegenerative diseases. Alarmingly, accelerated atrophy of the temporal lobes has strong connections to Alzheimer's disease stages, spotlighting the desperate need for early intervention.
This study not only serves as a wake-up call regarding the connection between heart health and cognitive decline but also challenges us to rethink healthcare strategies, particularly for men at higher cardiovascular risk. Will we heed this urgent call to action before it's too late?

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)