Discover How IL-37 Could Combat HPV-Induced Inflammation in Oral Epithelial Cells!
2024-12-30
Author: Siti
Introduction
Human Papillomavirus (HPV), one of the most common sexually transmitted infections globally, is notorious for its diverse manifestations and health implications. Characterized by its double-stranded DNA structure, HPV comprises over 200 distinct types, notably categorized into low-risk and high-risk strains, with the latter being linked to various cancers, including cervical, anal, and notably, head and neck cancers.
HPV and Inflammation
While the association of HPV with cancers is well-established, emerging studies reveal a significant connection between HPV and inflammatory responses in infected tissues. The complexity of this relationship suggests that HPV can provoke inflammation in host cells, which may, in turn, contribute to cancer progression. In patients with HPV-related cervical cancer, for example, heightened levels of inflammatory mediators, particularly interleukins like IL-6 and IL-8, have been observed, indicating a chronic inflammatory state that precedes malignancy.
Role of IL-37
Amidst these findings, researchers have turned their attention to a promising anti-inflammatory cytokine: Interleukin 37 (IL-37). This cytokine, part of the IL-1 family, is known for its potent ability to suppress inflammatory responses and maintain immune homeostasis. Prior investigations have shown IL-37's ability to dampen inflammation in various contexts, sparking interest in its potential role against HPV-induced inflammation, particularly in oral epithelial cells.
Research Study on IL-37
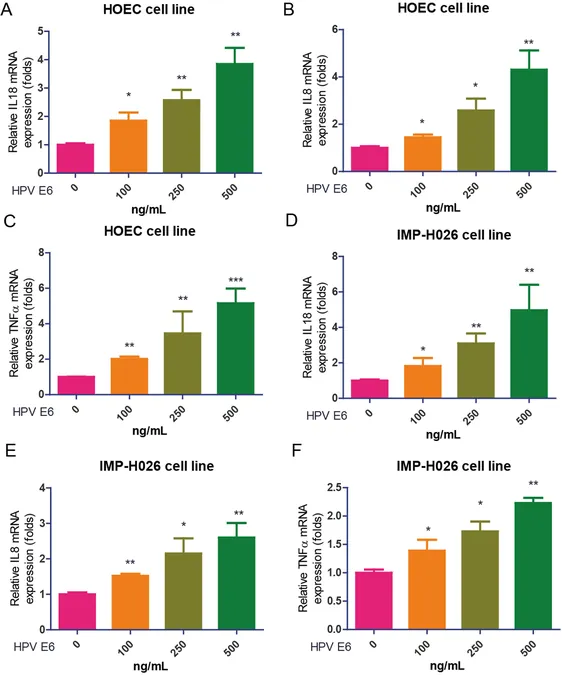
In a groundbreaking study involving two types of oral epithelial cells—HOEC and IPM-H026—researchers explored how HPV infection causes inflammation and how IL-37 might counteract this. They found that HPV E6 protein intensifies the expression of inflammatory markers such as IL-18, IL-8, and TNFα in these cells. Remarkably, co-treatment with IL-37 significantly lowered these inflammatory responses. The mechanism behind this protective effect appears to involve critical signaling pathways, notably the PI3K/AKT/mTOR pathway, which IL-37 seems to inhibit effectively.
Implications and Future Research
Recent data show that the patient's inflammation could be mitigated by targeting the PI3K pathway, and importantly, inhibitors of this pathway (like rapamycin) showcased a compromise in IL-37's efficacy, solidifying the notion that PI3K/AKT/mTOR signals play an essential role in regulating inflammation sparked by HPV in oral epithelial cells.
Moreover, the implications of HPV-induced inflammation are broad, linking chronic inflammation to cancer development. Therefore, understanding the regulatory effects of IL-37 on the HPV-driven inflammatory mechanisms could pave the way for new therapeutic strategies against HPV-related diseases, which are increasingly prevalent in various demographics, including those with healthy immune systems.
Conclusion and Limitations
However, this study is not without limitations. The findings were based solely on two types of oral epithelial cells, which may not fully encompass the complexities of oral tissues in vivo. Future research will be essential to confirm these results in more diverse populations and anatomical regions, as well as through in vivo models to validate the therapeutic potential of IL-37.
As HPV continues to pose considerable public health challenges worldwide, further exploration into IL-37 could lead to new avenues for prevention and treatment, offering hope to millions affected by HPV and its associated health threats.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)