Groundbreaking Discovery in Skin Renewal: How IL-38 Could Replace Animal Models in Research
2024-11-18
Author: Rajesh
In a remarkable scientific breakthrough, researchers have unveiled an unexpected mechanism that could change the landscape of skin renewal studies. The protein Interleukin-38 (IL-38), known for its critical role in regulating inflammatory responses, may serve as a new focal point in understanding skin health and disease.
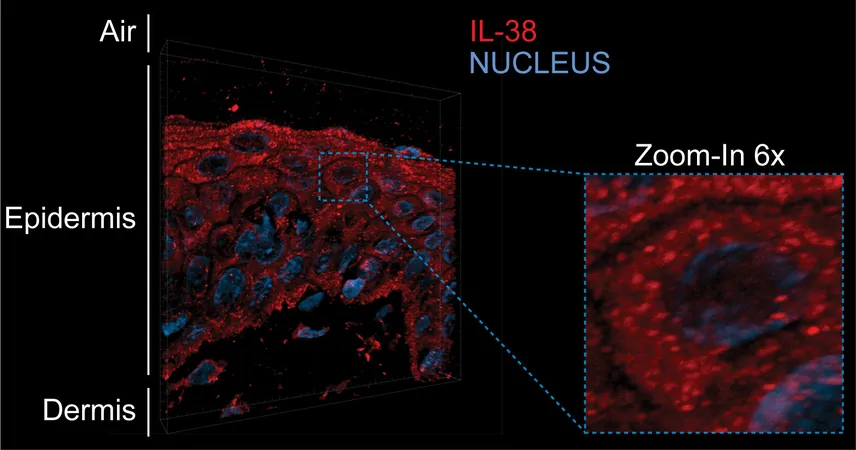
A dedicated team from the University of Geneva (UNIGE) has made an exciting discovery of IL-38 in condensates within keratinocytes—the vital cells that make up the epidermis. Moreover, they found that IL-38 levels are elevated near the skin surface where cells are directly exposed to atmospheric oxygen. This finding suggests a potential link to programmed keratinocyte death, a natural and essential process integral to skin turnover.
The study, published in the prestigious journal Cell Reports, offers fresh insights into human epidermis and its associated conditions. The outer layer of the skin acts as the body's first line of defense against environmental threats, and its renewal is largely powered by stem cells in the basal layer that generate new keratinocytes. As these cells rise to the skin's surface, they undergo differentiation and secrete protein condensates before undergoing programmed cell death—a process known as cornification—which culminates in a resilient barrier of dead cells.
Gaby Palmer-Lourenço, associate professor and principal investigator at UNIGE's Faculty of Medicine, emphasized, "While we have a good understanding of how the epidermis renews, the underlying mechanisms remain elusive."
IL-38: More Than Just a Signaler
Traditionally recognized for its anti-inflammatory properties, IL-38 has now revealed itself to play a vital role in keratinocyte behavior. "For the first time, we observed IL-38 forming condensates, specialized aggregates that suggest a distinct biochemical function," explained Palmer-Lourenço. Notably, the closer keratinocytes are to the epidermal surface, the more IL-38 these cells contain.
Oxidative Stress and Skin Renewal
Interestingly, the lack of blood vessels in the epidermis means that oxygen levels decrease as you move deeper into the skin. Increased oxygen levels at the surface come with a flip side: oxidative stress. This phenomenon causes the formation of harmful free radicals that threaten cell integrity.
According to Alejandro Díaz-Barreiro, the lead author of the study, "Our experiments demonstrate that oxidative stress can indeed trigger the condensation of IL-38, highlighting its role as a mediator in this process." The researchers hypothesize that as keratinocytes ascend closer to the epidermal surface, rising oxygen levels lead to an increase in protein condensates that signal the cells to undergo programmed death—essentially assuring the renewal cycle continues smoothly.
This hypothesis opens avenues for deeper investigations into the biology of epidermal renewal and could significantly enhance our understanding of skin diseases, such as psoriasis and atopic dermatitis.
Revolutionizing Research with Innovative Models
Moving forward, Alejandro Díaz-Barreiro expresses excitement about the future of their research. "In our previous model, we artificially induced oxidative stress in a single layer of keratinocytes, which does not accurately mimic natural conditions," he explains. The team is now developing a groundbreaking experimental system that introduces oxygen gradients to reconstituted human epidermis in vitro.
In this innovative model, only the very top layer of the skin will be exposed to oxygen, while the deeper layers remain sheltered. This cutting-edge approach promises a more accurate analysis of how oxidative stress influences epidermal renewal, ultimately providing a sophisticated alternative to traditional animal models that have long been the standard in skincare research.
As we stand on the brink of this significant shift in medical research, the implications of effectively studying skin biology without relying on animal models could be monumental. This can not only transform our approach to dermatological studies but also could lead to groundbreaking advancements in therapies for various skin conditions.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)