Groundbreaking Discovery Links Mitochondrial Dysfunction to Crohn's Disease and Offers Hope for New Treatments!
2024-10-11
Author: Mei
Breakthrough Overview
Researchers at the Technical University of Munich (TUM) have made an astonishing breakthrough in understanding Crohn’s disease, showcasing how dysfunctional mitochondria can severely impact the gut microbiome. This significant finding, published in the prestigious journal *Cell Host & Microbe*, underlines the critical role mitochondria play not only in cellular energy production but also in the complex interaction with the gut microbiome.
Understanding Crohn’s Disease
Crohn’s disease is characterized by debilitating symptoms such as chronic diarrhea, intense abdominal pain, and fever, yet the exact causes remain largely elusive. However, a pattern has emerged in recent years: changes in the gut microbiome often correlate with inflammatory diseases like Crohn’s, prompting researchers to investigate further into these microbial alterations.
Research Insights
A dedicated team led by Dirk Haller, the chair of nutrition and immunology at TUM, has delved into the intricacies of the microbiome, the intestinal epithelium— a critical tissue layer that processes nutrients and protects against pathogens— and mitochondrial function. Their research reveals that mitochondrial dysfunction can significantly disrupt the composition of the microbiome, leading to the inflammatory responses characteristic of Crohn's disease.
Innovative Methodology
The research team's hypothesis was that mitochondria do more than just serve as the cell’s powerhouses; they also interact closely with gut bacteria. Previous studies had already indicated that patients suffering from chronic intestinal inflammation exhibit markers of mitochondrial stress, pointing towards a potential link.
Mice Model Experimentation
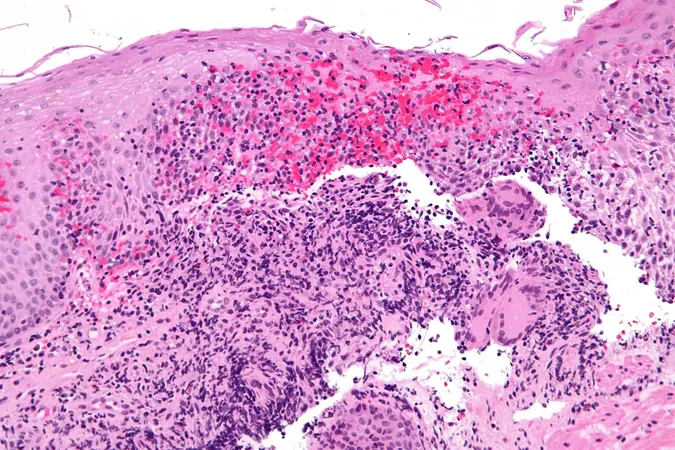
In an innovative approach, the researchers engineered mice to disrupt mitochondrial function by removing a gene responsible for producing the essential protein Hsp60, crucial for mitochondrial activity. This manipulation resulted in tissue damage within the intestinal epithelium that mimicked the injuries observed in Crohn’s patients, along with gene activation changes typically seen in various stages of the disease. Intriguingly, the gut microbiome adapted to these mitochondrial disruptions, undergoing significant compositional changes.
Causal Relationship Established
For the first time, this study establishes a direct causal relationship between mitochondrial dysfunction and tissue damage in the intestines, alongside disease-related changes in the gut microbiome. Remarkably, these findings open the door for potential new therapies for individuals battling inflammatory conditions.
Future Implications
Currently, treatment strategies for Crohn’s disease primarily focus on symptom management through anti-inflammatory medications. However, Haller expresses an optimistic vision for the future: 'We hope to discover new active substances that can restore the functionality of impaired mitochondria, essentially facilitating their repair. This may significantly curb the intestinal damage that serves as a precursor for chronic inflammatory processes.'
Broader Impact
The implications of this research extend far beyond Crohn’s disease, suggesting that drugs targeting mitochondrial pathways or the interplay between the microbiome and mitochondria could revolutionize treatment approaches for various inflammatory conditions. The journey toward understanding and potentially curing Crohn’s disease is now more promising than ever, as science continues to unlock the mysteries of our body's intricate systems!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)