Revolutionary Peptide-Enhanced Nanoparticles Set to Transform mRNA Delivery for Neurological Treatments
2024-12-17
Author: Nur
Revolutionary Peptide-Enhanced Nanoparticles Set to Transform mRNA Delivery for Neurological Treatments
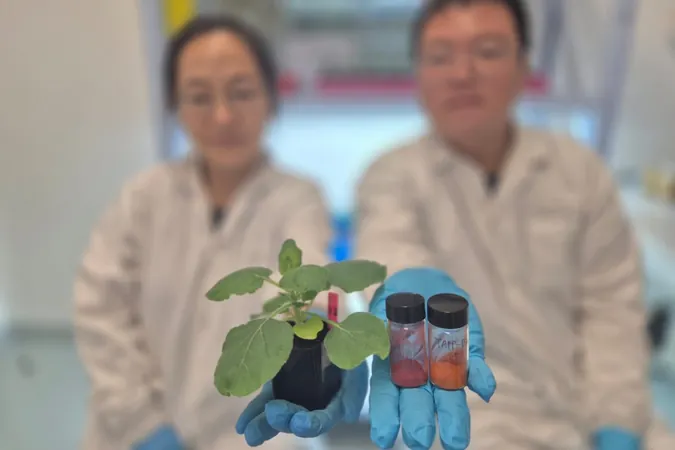
In a groundbreaking advancement from the University of Pennsylvania’s School of Engineering and Applied Science, engineers have successfully modified lipid nanoparticles (LNPs) to not only breach the formidable blood-brain barrier (BBB) but also deliver mRNA directly to specific cell types, particularly neurons. This innovative research, documented in the recent publication “Peptide-Functionalized Lipid Nanoparticles for Targeted Systemic mRNA Delivery to the Brain” in the journal Nano Letters, paves the way for novel mRNA therapies aimed at combatting neurological conditions such as Alzheimer’s disease and Parkinson’s disease.
The team identified peptides as precision-targeting agents capable of guiding LNPs to endothelial cells lining the brain's blood vessels and to the neurons themselves. This represents a crucial leap in ensuring that mRNA treatments reach the appropriate locations for effective therapeutic action.
Previously, researchers had established that LNPs could navigate the BBB and introduce mRNA into the brain, but control over specific cell targeting remained an elusive goal. “Our earlier work was primarily a proof-of-concept,” explained Dr. Michael J. Mitchell, the paper's senior author. “We demonstrated the possibility of delivering a package from Pennsylvania to California, but without addressing its final destination within California. Now, with the introduction of peptides, we can strategically direct the package to locations with shared characteristics—imagine sending it to every house with a red mailbox.
The Challenge of the Blood-Brain Barrier
The BBB poses significant challenges for drug delivery due to its function as a selective permeability barrier designed to exclude harmful substances, including most pharmaceutical compounds. Notably, mRNA molecules are often too large to cross this barrier. Conventional approaches often involve invasive strategies such as direct injections into the brain or spinal column, which carry their own set of risks.
The scientists leveraged a surprising insight: certain formulations of LNPs, composed of lipids akin to those naturally found in dietary oils, possess the capability to slip through the BBB due to their fat-soluble nature—similar to the way alcohol and THC can impact the brain.
Traditionally, research on organ-targeting with LNPs focused heavily on using antibodies to enable specificity. However, the study highlighted a significant drawback to this approach; the larger size of antibody-coated LNPs complicates BBB penetration. In contrast, peptides, which are considerably shorter than antibodies, can be integrated into LNPs more efficiently. They are not only cheaper to produce but also exhibit reduced likelihood of causing instability or immune reactions.
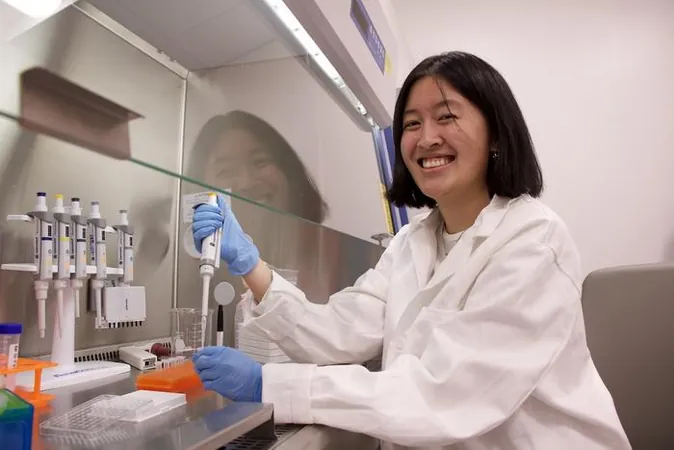
The inspiration for this peptide application arose unexpectedly when doctoral student Emily Han encountered a bat, leading her to investigate the mechanisms behind rabies virus transmission across the BBB. She discovered a promising peptide called RVG29, which is derived from the glycoprotein of the rabies virus.
To ensure the success of their method, the researchers meticulously confirmed the binding of peptides to LNPs, developing quantification techniques to distinguish the peptides within the complex mixture of materials in LNPs. Following this, they undertook a rigorous examination in animal models to confirm that peptide-functionalized LNPs (pLNPs) reached their designated neuron targets.
The labor-intensive process involved the disassembly of brain tissues to study cellular interactions—an endeavor that took over six months of meticulous preparation.
Looking Ahead: The Threshold for Therapeutic Efficacy
Hudging closer to clinical applications, the research team is now poised to explore a pivotal question in the realm of neurotherapeutics: how many neurons need to be targeted to achieve meaningful clinical improvement or possibly a cure? The analogy used by Mitchell highlights this inquiry well: "Do we need to deliver to every house with a red mailbox, or will addressing just 10% suffice?”
This crucial understanding will guide future methodologies, sharpening the focus of mRNA therapies for neurodegenerative conditions. As this journey unfolds, the prospect of effective, non-invasive treatments for serious brain diseases inches ever closer to reality, driven by the innovation of peptide-guided LNPs.
Stay informed on this monumental advancement—who knows, it might just change the future of brain health!

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)