Rising Challenges of Drug-Resistant Tuberculosis in Cameroon: Key Insights from a 10-Year Study
2024-11-18
Author: Wei Ling
Introduction
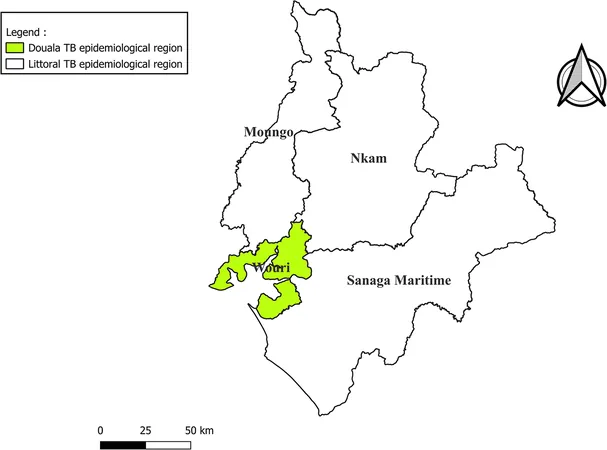
Tuberculosis (TB) continues to pose a significant global health threat, particularly in regions like Cameroon, where the specter of drug resistance adds urgency to treatment strategies. According to recent data, the prevalence of drug-resistant TB (DR-TB) in Cameroon stood at 1.4% among new cases and alarmingly high at 8.3% among those undergoing retreatment in 2022. This retrospective study, spanning a decade from 2013 to 2022 in the Littoral region of Cameroon, provides critical insights into the trends in DR-TB, treatment outcomes, and the risk factors contributing to unfavorable treatment responses.
Study Overview
Our comprehensive analysis utilized data from a DR-TB database, assessing quality through various indicators, including zero-reporting, completeness, consistency, and validity. We distinguished DR-TB cases into categories such as Rifampicin-resistant TB (RR-TB), multi-drug resistant TB (MDR-TB), pre-extensive drug-resistant TB (pre-XDR-TB), and extensively drug-resistant TB (XDR-TB), employing descriptive statistics to interpret the data.
Key Findings
Between 2013 and 2022, a total of 567 DR-TB cases were documented in the Littoral region. The data revealed a median age of 34 years among patients, with a male-to-female ratio of 3:2. The years 2013 to 2018 witnessed a concerning rise in case reporting, culminating in a peak in 2018. However, the overall treatment outcomes were concerning: while 60.8% were cured, 26.4% completed treatment, and dishearteningly, 7.2% succumbed to the disease, highlighting the urgent need for intervention.
The demographics of the patients indicated that 52% of the deaths occurred among those who initially refused treatment, with 20% of deaths occurring within the first month of therapy. Notably, life-threatening co-infections with HIV were found in 15.5% of deceased patients.
Risk factors were identified that significantly influenced poor treatment outcomes. Males were 2.5 times more likely to experience negative outcomes than females, while a positive HIV status increased risk by a factor of 2.1. Previous cases of DR-TB conferred an even greater risk, at 3.9 times.
Conclusion
The data projects a concerning trajectory for DR-TB in the Littoral region of Cameroon, indicating serious public health challenges. Despite an overall treatment success rate of 87.2%, stark disparities remain, urgently calling for improved strategies. Key recommendations include universal drug susceptibility testing, proactive patient education to mitigate treatment refusal, and thorough pre-treatment counseling to enhance patient adherence.
In the broader context, TB remains the second leading infectious killer worldwide, and addressing its rising drug resistance is critical. The findings from this study can significantly inform public health policies and contribute to achieving the World Health Organization’s goal of eliminating TB by 2030.
As global health authorities continue to grapple with TB management, the experience from Cameroon serves as a stark reminder of the complexities surrounding drug resistance and the pressing need for coordinated efforts to protect vulnerable populations. With the looming threat of further resistance, the time for action is now.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)