Shocking Link Revealed: Catastrophic Health Expenses and Rising Depression Rates Among China's Elderly!
2025-04-08
Author: Yu
Introduction
Depression has emerged as a leading mental health epidemic worldwide, resulting in severe challenges for individuals, families, and health systems alike. Among the elderly, particularly in rapidly aging nations like China, the situation is dire. The prevalence of depression in older Chinese adults has soared, with estimates suggesting alarming rates between 17.4% and 46.15%. As we navigate the complexities of an aging population, acknowledging the factors that exacerbate this mental health crisis is vital.
The Hidden Financial Burden
A significant yet often overlooked contributor to mental health deterioration is catastrophic health expenditure (CHE). CHE occurs when out-of-pocket medical expenses exceed a certain threshold of a household's financial capacity, leading to unbearable financial stress. Globally, over 200 million people are affected by CHE, pushing many into poverty. In China, although rates of CHE have slightly decreased from 13.58% in 2010 to 11.06% in 2016, the situation remains precarious. For the elderly, who are particularly vulnerable, the financial strain from CHE can amplify feelings of isolation, depression, and anxiety.
Economic Disparities and Mental Health
Recent studies illuminate the overwhelming impact of socio-economic factors on mental health outcomes. Low-income individuals are disproportionately affected by mental disorders, while higher-income households tend to have better access to healthcare and fewer financial burdens. Economic hardship not only induces psychological stress but may escalate to severe mental health issues, particularly in vulnerable populations like the elderly. Researchers highlight the interconnectedness of economic distress and mental health decline, suggesting that those with low income and limited social engagement face the highest risks.
The Power of Social Engagement
What’s intriguing is the role of social activities in mitigating these mental health impacts. Findings show that participation in social activities can foster emotional support and resilience, thereby cushioning the adverse effects of CHE. Engaging in social interactions enhances one's well-being, reduces feelings of isolation, and increases overall quality of life. This interaction between mental health and social involvement is crucial, especially for elderly individuals facing upheaval from health expenditures.
Study Insights: Evidence from China
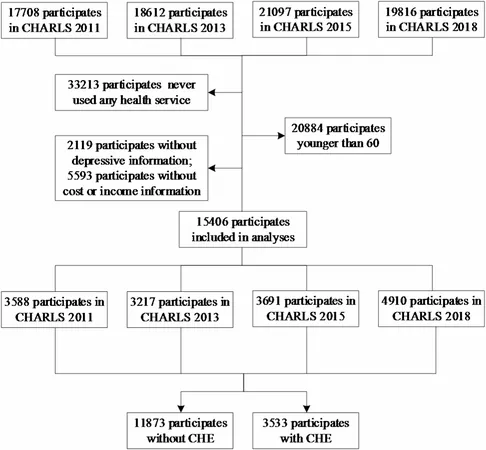
This study harnesses data from the Harmonized China Health and Retirement Longitudinal Study, focusing on 15,406 individuals aged 60 and above. The results reveal a concerning pattern: elderly individuals experiencing CHE report significantly higher levels of depressive symptoms, especially among low-income or socially inactive groups. Those without social engagement demonstrated a stark contrast in mental health outcomes compared to those who actively participated in community activities.
Key Findings and Implications
1. CHE and Depression Connection: The study firmly establishes that CHE correlates with increased depressive symptoms in the elderly. Financial hardships associated with health expenditures introduce a psychological burden that can lead to chronic mental health issues.
2. Moderating Effects of Income and Social Activity: Analysis suggests that economic conditions and social engagement significantly moderate the relationship between CHE and depression. Elderly individuals with lower incomes and little to no participation in social activities are at greater risk, illustrating the critical nature of both financial stability and community interaction.
3. Recommendations for Policy Reform: To combat these dual challenges, policymakers must fortify existing healthcare supports and integrate mental health resources more comprehensively into healthcare systems. Enhanced financial protections, particularly for low-income households, and increased access to mental health services are vital. Community initiatives encouraging social engagement should also be prioritized, providing elderly individuals with opportunities for connection and support.
Conclusion: A Call to Action
This research underscores an urgent need for targeted interventions to address the impacts of catastrophic health expenditures on mental health among China’s elderly. When financial and social support systems align, we can alleviate the burdens of depression and foster a healthier, more resilient aging population. Moving forward, it is essential that we transform insights into actions that not only improve financial stability but also enhance emotional well-being and community connection for our elderly citizens. The time for change is now!




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)