Survival Struggles: What Predicts Outcomes for Perforated Peptic Ulcer Patients in Ethiopia?
2025-04-12
Author: Li
Understanding the Grave Stakes of Perforated Peptic Ulcers
Perforated peptic ulcer (PPU) represents a dire surgical emergency that poses a high risk of mortality and serious complications. Despite various studies, there's a notable absence of comprehensive data on the management and outcomes of this critical condition in Ethiopia. This systematic review endeavors to illuminate the mortality and complication rates stemming from PPU treatments, alongside identifying key risk factors contributing to these outcomes.
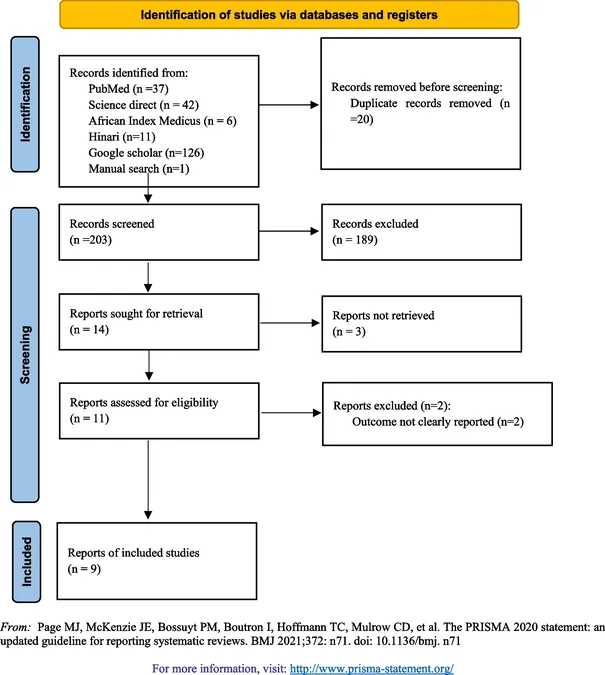
Thorough Research Leading to Crucial Insights
A meticulous search across databases such as PubMed, Science Direct, and local university libraries allowed researchers to gather a wealth of information. Data was extracted and analyzed using sophisticated statistical software, revealing a shocking mortality rate of 6.68% and complication rate of 23.21% among Ethiopian patients treated for PPU. Alarmingly, patients presenting more than 24 hours after symptoms appeared exhibited four times the odds of encountering complications compared to those who sought timely medical attention.
Key Findings: Predictors of Complications and Mortality
The analysis discovered that specific factors significantly influenced health outcomes. Patients with low systolic blood pressure faced nearly five times higher risks of complications. The review underscores that delays in seeking surgical intervention and demographic factors like age substantially affect post-treatment recovery. Understanding these predictors is crucial, not just for individual patient care, but for improving health policies and clinical practices in combating PPU.
The Bigger Picture: Global Context and Local Challenges
Globally, peptic ulcer disease affects around 8 million individuals annually, with unfortunate complications leading to emergency surgeries. Unfortunately, in resource-limited settings like Ethiopia, barriers including limited healthcare access exacerbate the challenges faced by patients. While this study paints a comparative picture revealing lower mortality rates in Ethiopia than in other parts of Sub-Saharan Africa or high-income countries, the need for better healthcare infrastructure and prompt intervention becomes glaringly clear.
Urgent Call to Action: Enhancing Patient Outcomes in Ethiopia
With findings indicating that simple measures like early emergency care can drastically change outcomes, the call for public health initiatives is loud and clear. Increasing awareness about PPU symptoms and prioritizing timely surgical responses could save lives. Furthermore, addressing the existing gaps in healthcare provision and surgical resources will be vital steps toward reducing PPU-related mortality and morbidity in Ethiopia.
Conclusion: Knowledge is Power
This study not only provides essential data on the treatment of perforated peptic ulcers but also identifies critical areas for intervention. By sharpening focus on early diagnosis, intervention, and management strategies specific to risk factors, healthcare providers can improve survival rates and quality of life for patients facing this severe condition. It's a pivotal moment for Ethiopian healthcare—one that demands immediate action and sustained commitment.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)