Unlocking the Mystery: Fasting Plasma Glucose to HDL Cholesterol Ratio as a Game-Changer for NAFLD Detection
2025-04-09
Author: John Tan
Introduction to a Revolutionary Biomarker
Researchers are shining a spotlight on the fasting plasma glucose to high-density lipoprotein cholesterol ratio (FHR) as a groundbreaking tool not just for cardiovascular disease, but also for predicting non-alcoholic fatty liver disease (NAFLD). This study dives deep into the potential that FHR holds for revolutionizing NAFLD detection.
Study Overview: Methods and Findings
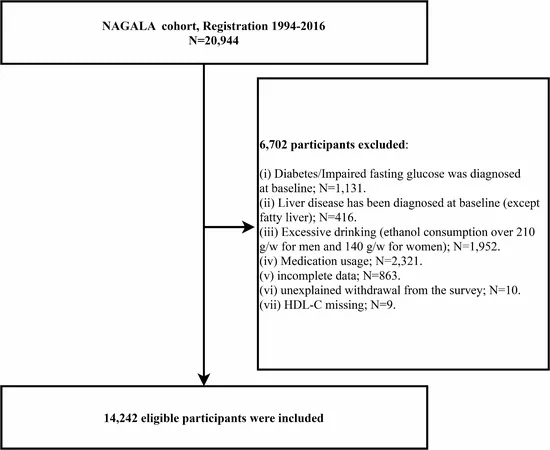
In this comprehensive analysis, data from over 14,000 health examination participants were scrutinized. Through advanced statistical methods like restricted cubic spline regression and multivariable logistic regression, the researchers uncovered a significant link between elevated FHR levels and NAFLD. Remarkably, those in the highest FHR quartile showed a staggering 134% increased risk of NAFLD compared to the lowest quartile.
The Rising Threat of NAFLD
NAFLD is not just a medical term; it’s the most common chronic liver disease worldwide, associated with serious health issues like cirrhosis and liver cancer. Recent trends reveal an alarming 50% increase in global NAFLD prevalence over the past three decades, with nearly 40% of people affected between 2016 and 2019. This makes identifying individuals at risk more crucial than ever.
Current Diagnostic Challenges
While liver biopsies are the gold standard for diagnosing NAFLD, their invasive nature and cost make them impractical for large-scale screening. Presently, NAFLD diagnosis relies heavily on alcohol consumption history and ultrasound imaging, which, while effective, could benefit from less invasive alternatives.
FHR: A Potential Game-Changer
FHR combines fasting plasma glucose and HDL cholesterol to create a comprehensive index that may enhance risk stratification for NAFLD. Elevated fasting plasma glucose levels are closely linked to liver fat accumulation, while HDL cholesterol plays a vital role in reducing this burden. The innovative combination of these two measurements could lead to earlier and more accurate detection of NAFLD.
What the Numbers Reveal
The research unveiled a intriguing finding: those with FHR levels above 3 experienced a significant increase in NAFLD prevalence. The analysis highlighted a critical threshold of 3.89 for optimal NAFLD identification, showcasing FHR's superiority over traditional metrics.
Implications for Future Research and Practice
The study suggests that incorporating FHR into routine assessments could transform how healthcare providers identify NAFLD and potentially mitigate its rise across global populations. As metabolic health becomes a pressing public health concern, FHR could prove invaluable in mitigating the mounting burden of chronic diseases.
Conclusion: A Bright Future Ahead for NAFLD Detection
The FHR index represents a promising leap forward in non-invasive NAFLD diagnosis, allowing for timely interventions that could save lives. As researchers continue to validate these findings, the integration of FHR into clinical practice may soon become a standard for managing liver health.



 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)