Urgent Findings on Central Line-Associated Bloodstream Infections (CLABSI) in Palestine's Intensive Care Units: A Call for Better Practices
2025-04-03
Author: Nur
Introduction
Central line-associated bloodstream infections (CLABSIs) are alarming complications arising from the use of central venous catheters (CVCs). With an incidence rate of approximately 4.1 per 1,000 central line days, these infections lead to longer hospital stays, higher healthcare costs, and increased mortality rates. Each year, the United States witnesses around 250,000 bloodstream infections, significantly tied to intravascular devices. In intensive care units (ICUs), the average CLABSI rate hovers around 0.8 per 1,000 catheter days, while countries like North India report rates as high as 17.04 per 1,000 catheter days. Comparatively, high-income countries like China report lower rates, around 1.50 per 1,000 catheter days.
Impact of CLABSI
A meta-analysis has revealed that patients with CLABSIs face a 2.75 times higher risk of dying while hospitalized compared to those without such infections. Fortunately, many of these infections could be prevented if healthcare professionals adhere to evidence-based guidelines. Following protocols such as thorough handwashing, implementing full-barrier precautions during catheter insertion, disinfecting the skin with chlorhexidine, and timely catheter removal can dramatically reduce incidence rates.
Study Background
In Palestine, however, information concerning CLABSI prevalence and characteristics among ICU patients is limited. Our recent study conducted at An-Najah National University Hospital aimed to address this gap, examining the factors influencing CLABSI occurrences in ICU patients from 2018 to 2022.
Methodology
The methodology involved a retrospective observational chart review of adult patients who underwent CVC insertion. Using the Seldinger technique and maintaining aseptic conditions, the data collected included demographic details, comorbid conditions, catheter types, and rates of causative organisms in cases where CLABSI was confirmed.
Results
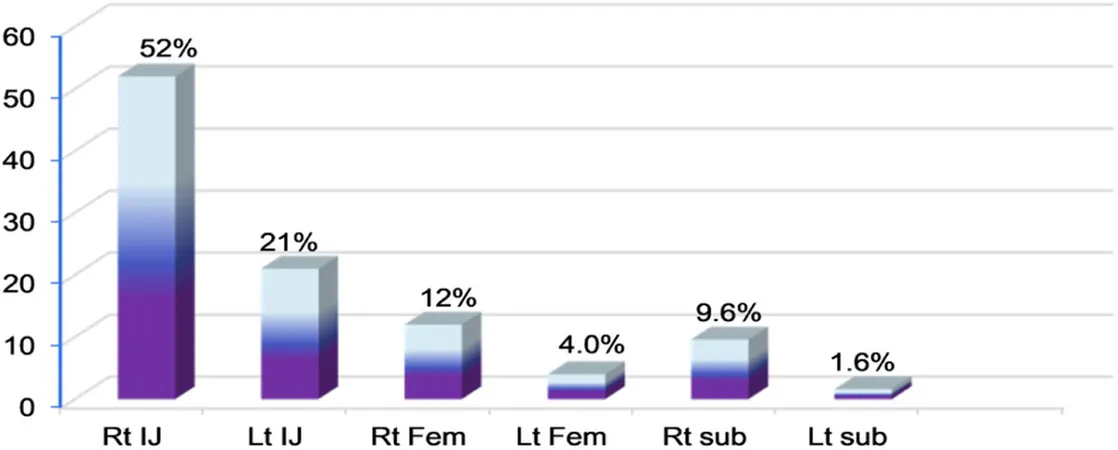
Results from examining 323 patients revealed that the incidence of CLABSI stood at around 5.9%, with a CLABSI rate of approximately 8.91 per 1,000 device days—an alarming statistic when viewed against international benchmarks. The average age of patients was 52 years, and common conditions included diabetes and hypertension. Mortality rates were found to be 33%.
Microbial Findings
A significant finding was that the most frequently isolated bacteria were Acinetobacter baumannii and Staphylococcus haemolyticus, both associated with higher risks of complications. Notably, 10% of CLABSI patients had previous COVID-19 infections, suggesting a potential link between the pandemic and increased susceptibility to infections.
Adherence to Prevention Guidelines
Despite the increase in CLABSI rates, adherence to prevention guidelines appears inadequate. Factors such as increased CVC utilization ratios and multiple catheter insertions were significant predictors of infection risk. Unfortunately, key data on healthcare practices, such as nurse-to-patient ratios and strict compliance with hygiene protocols, were not collected in this study, leaving potential gaps in the analysis.
Conclusion
This study reveals a concerning need for heightened awareness and training among healthcare staff in Palestine to ensure better adherence to infection control practices. With the rising incidence of CLABSI, especially linked to underlying comorbidities, a reassessment of current medical protocols appears critically necessary. As healthcare professionals, policymakers, and researchers continue to strive for improved outcomes in critical care settings, the findings from this study demand urgent attention. It is clear that investing in enhanced training and equipment, fostering compliance with established infection control guidelines, and investigating the factors contributing to high CLABSI rates can ultimately reduce these preventable infections in Palestine.




 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)