Revolutionary New Allergy Test Set to Change Lives!
2024-10-15
Author: Noah
In a groundbreaking discovery, researchers at the University of Bern and Bern University Hospital have unveiled a revolutionary test designed to streamline the diagnosis of allergies, with its efficacy particularly validated for peanut allergies among children and adolescents. This advancement promises not only to enhance clinical practices but also significantly reduce the burden of food allergies on families and healthcare systems globally.
Food allergies are becoming an alarming public health crisis, affecting up to 10% of the population in certain regions, predominantly impacting young children. Among these allergies, peanut allergy stands out due to its frequency and the severity of reactions, which can often be life-threatening.
The emotional and physical stress caused by food allergies extends beyond the individual; it can ripple through family dynamics and strain healthcare resources. Currently, the oral food challenge—where patients consume the allergen under medical supervision—remains the gold standard for allergy diagnosis but carries considerable risks and complexity. Alternatives such as skin prick tests and blood tests often yield inaccurate results, leading to misdiagnosis and unnecessary dietary restrictions.
Under the direction of Prof. Dr. Alexander Eggel, along with Prof. Dr. Thomas Kaufmann, a dedicated team of researchers has developed an innovative test in 2022 that simulates allergic reactions in vitro, providing an accessible alternative to existing methodologies. Their recent clinical research, alongside esteemed colleagues from the Hospital for Sick Kids in Toronto, has confirmed the test's effectiveness using samples from individuals with verified peanut allergies.
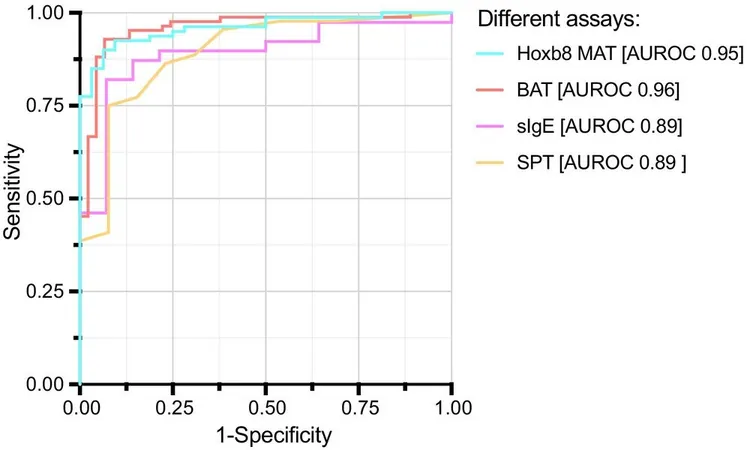
The pioneering test, known as the Hoxb8 Mast Cell Activation Test (Hoxb8 MAT), represents a significant leap forward. As explained by Eggel, the process involves sensitizing laboratory-cultured mast cells with serum from allergic patients, which then respond to varying concentrations of allergens without the need for patients to ingest any potentially dangerous substances.
In a study involving 112 pediatric participants, the new test exhibited an astonishing diagnostic accuracy rate of 95%, outstripping traditional methods such as IgE antibody measurement and skin prick testing. The rapid results—processed within just two days—underscore the test’s practicality and efficiency.
This innovative approach not only minimizes false negatives but also integrates multiple parameters critical to understanding allergic reactions. Moreover, the use of stable blood serum simplifies the logistics of testing, as samples can be easily collected and stored, overcoming significant barriers present in previous diagnostic methods.
The ramifications of this discovery extend far beyond peanut allergies; the technology holds promise for diagnosing a variety of food allergies, potentially transforming lives for millions affected globally. As Eggel aptly concludes, this advancement exemplifies the remarkable journey from fundamental research to clinical application, ushering in an era where allergy management can be dramatically simplified for patients and healthcare providers alike.
This breakthrough is not just a test; it is a beacon of hope for countless families grappling with the challenges of food allergies.








 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)