Understanding the Deadly Impact of Surgical Delays on Breast Cancer Patients: A Closer Look at Subtypes
2024-12-31
Author: John Tan
Introduction
Breast cancer remains a leading health concern for women in the United States, with advancements in detection technology ensuring that a staggering 66% of cases are diagnosed at localized stages, where surgical intervention is most effective. Yet, despite these advancements, the battle is far from over. Research indicates that treatment delays significantly heighten mortality risks, revealing a complex interplay between surgery timing and breast cancer subtypes.
The Hidden Risks of Treatment Delays
A comprehensive meta-analysis encompassing over a million patients with various solid tumors, including breast cancer, has confirmed that the risk of death increases by 6-8% for every four-week delay in receiving treatment. Breast cancer patients, particularly those diagnosed at earlier stages, must navigate the additional peril of increased risk with prolonged time to surgery (TTS). A groundbreaking quality measure introduced by the Commission on Cancer (CoC) now mandates that accredited facilities provide surgical interventions within 60 days of diagnosis to combat this issue.
The Subtype Dilemma
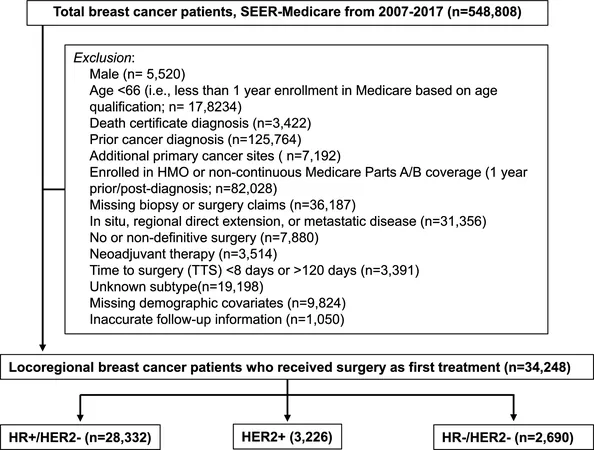
Current research underscores the importance of understanding how different breast cancer subtypes react to these surgical delays. A retrospective study that analyzed the outcomes of over 350,000 patients has shown a consistent increase in overall mortality risk associated with TTS — yet, these risks manifest differently across subtypes. In patients with hormone receptor-positive (HR+) and HER2-negative breast cancer, mortality risk surged dramatically after an initial 42-day waiting period. On the contrary, those with HER2-positive and triple-negative breast cancer experienced a more linear increase in risk.
Interestingly, the growing trend of surgical delays appears to disproportionately affect Black patients, who face extended TTS compared to their White counterparts. The implications of such disparities are alarming and necessitate a concerted effort to address healthcare inequalities.
Statistical Insights
In this innovative study harnessed from the SEER-Medicare database, patients diagnosed between 2010 and 2017 were scrutinized to understand how TTS affected breast cancer-specific mortality (BCSM). The results were telling: the adjusted cumulative incidence of BCSM steadily increased across all subtypes with longer waiting times. Specifically, patients with HR+/HER2- subtype showed alarmingly steep exponential spikes in mortality risk, with a staggering 3% higher projected mortality rate at a TTS of 120 days compared to just 30 days.
The research also adeptly employed advanced statistical models to capture the nuanced relationships between surgical delays, subtype characteristics, and mortality outcomes, revealing that patients with HR+ tumors faced a dire trajectory regarding their health during extended waiting periods.
The Road Ahead
These findings not only highlight the critical need for timely surgical interventions but also encourage further investigation into the biological mechanisms that may cause discrepancies in treatment outcomes based on breast cancer subtypes. Understanding whether delayed treatment allows for tumor progression or other changes in biology could offer vital insights for optimizing patient care strategies.
As we push forward in the battle against breast cancer, prioritizing swift surgical responses and tackling systemic healthcare disparities must become imperative. Patients deserve a fighting chance against this pervasive disease, and knowledge coupled with strategic action can pave the way for improved outcomes across all demographics.
Conclusion
In summary, this study brings to light the pressing issues surrounding surgical delays in breast cancer treatment, particularly the variances in associated mortality risks by subtype. As we adopt a more nuanced understanding of these relationships, our approach to patient care must transform to ensure that all women can access timely and appropriate interventions.

 Brasil (PT)
Brasil (PT)
 Canada (EN)
Canada (EN)
 Chile (ES)
Chile (ES)
 Česko (CS)
Česko (CS)
 대한민국 (KO)
대한민국 (KO)
 España (ES)
España (ES)
 France (FR)
France (FR)
 Hong Kong (EN)
Hong Kong (EN)
 Italia (IT)
Italia (IT)
 日本 (JA)
日本 (JA)
 Magyarország (HU)
Magyarország (HU)
 Norge (NO)
Norge (NO)
 Polska (PL)
Polska (PL)
 Schweiz (DE)
Schweiz (DE)
 Singapore (EN)
Singapore (EN)
 Sverige (SV)
Sverige (SV)
 Suomi (FI)
Suomi (FI)
 Türkiye (TR)
Türkiye (TR)
 الإمارات العربية المتحدة (AR)
الإمارات العربية المتحدة (AR)